Osteoporosis can cause receding gums, decreased grip strength, and pain in the neck or back. Consult a physician if you think you may have osteoporosis. To confirm your diagnosis, they can run a bone density test.
Your bones will become thinner, weaker, and more brittle if you have osteoporosis. The International Osteoporosis Foundation reports that 6.3 percent of men and 21.2 percent of women over 50 are affected worldwide.
Your bones are made of living tissue, which constantly breaks down and rebuilds itself despite their extreme strength. Your body can replace lost bone tissue more quickly than it can break down new bone up until the early 20s. But as you age, this process slows down.
Old bone tissue may degrade more quickly as you get older than it grows. Osteoporosis can follow from this, making your bones more brittle and porous and raising your risk of bone fractures.
Knowing the signs and risk factors will help you maintain strong bones for the rest of your life.
Table of Contents
Symptoms of osteoporosis

The best way to avoid some of the more catastrophic effects of osteoporosis, including bone soreness or fractures, is to treat it as soon as possible.
What kinds of symptoms, then, should you watch out for, and when do they appear? Let’s examine the symptoms of osteoporosis in its early and later phases in more detail.
Signs and symptoms of early-stage osteoporosis
Rarely are there early, noticeable symptoms of bone loss. Many times, people are unaware of their weak bones until they suffer a break in their wrist, hip, or another bone.
But several indicators and symptoms, like the following, may suggest possible bone loss:
- receding lips. Should your jaw be losing bone, your gums may retreat. Request a jaw bone loss screening from your dentist.
- reduced force in the grasp. Low handgrip strength was associated with low bone mineral density, according to research on postmenopausal women and total bone mineral density. Furthermore, having weaker grip strength can make you more likely to fall.
- Fingernails weak and brittle. Strength of nails might indicate bone health. However, you should also be aware of other elements that could have an impact on your nails, like exposure to extreme heat or cold, frequent use of acrylic nails or nail polish remover, or prolonged immersion in water.
Osteoporosis typically doesn’t create many early symptoms, aside from changes in bone density. Consult your physician or other healthcare provider as soon as possible to catch it in its early stages, particularly if you have a family history of osteoporosis.
Signs and symptoms of later-stage osteoporosis
When bone mass continues to decline, you might begin to exhibit more overt signs like:
- Reduction in height. You may get shorter as a result of spinal compression fractures. One of the most obvious signs of osteoporosis is this.
- break caused by a fall. One of the most typical indications of brittle bones is a fracture. Broken bones can result from falls or even small movements like stepping off a curb. Strong coughs or sneezes can potentially cause some osteoporosis fractures.
- Neck or back ache. Spinal compression fractures can result from osteoporosis. Because the crushed vertebrae may constrict the nerves that extend from the spinal cord, these fractures can be extremely painful. From mild soreness to incapacitating pain, the pain sensations might vary greatly.
- Hunched over or broken. A small curvature of the upper back may also result from the vertebrae being compressed. Kyphosis is a stooped back that can hurt the neck and back. Because of the increased airway pressure and constrained lung expansion, it may even impair breathing.
Which factors put one at risk for osteoporosis?

Although osteoporosis can affect both men and women, it primarily affects women due to changes in hormones brought on by age.
Typical osteoporosis risk factors include:
- advanced age
- experiencing menopause before to the age of 45
- undergoing ovarian excision prior to age 45
- low levels of testosterone in males
- being low in estrogen in females
- taking certain drugs that cause hormone levels to drop
- cigarette smoking
- having osteoporosis in their family
- frequent alcohol consumption
- not engaging in enough regular physical activity, especially walking or other weight-bearing exercises
Osteoporosis is more common in Caucasian and Asian individuals, particularly in women, according to study (Reliable Source).
You may be more susceptible to osteoporosis if you have certain medical issues. Among these are:
- renal malfunction
- inadequate levels of vitamin D
- glucose ,
- hyperthyroidism and diabetes
- elevated parathyroid hormone
- dementia
- rheumatoid arthritis
- a history of breast cancer
- fibrosis cystica
- the sickle cell disease
- celiac disease or inflammatory bowel disease-related malabsorption
Osteoporosis risk can also be increased by immunosuppressive drugs and steroids such as prednisone. Additionally, if the dosage of thyroid replacement therapy is too high, seizure drugs may also raise this risk.
How does one diagnose osteoporosis?
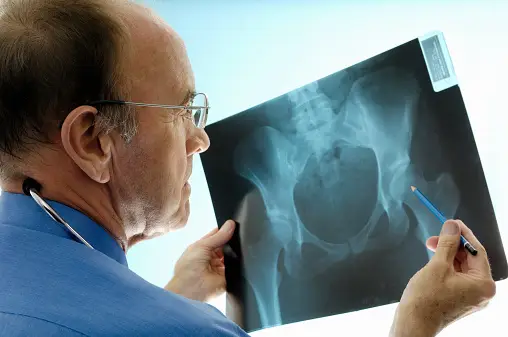
Your doctor may use a bone density test to identify osteoporosis. To find out how dense your bones are in comparison to those of persons your age and gender, a device known as a dual energy X-ray absorptiometry, or DXA machine, can scan your hips and spine.
The principal means of diagnosis is the DXA scan. It can take ten to fifteen minutes to complete the test.
An additional imaging modality that physicians may employ to identify or validate an osteoporosis diagnosis is ultrasonography, typically focused on the patient’s heel.
In accordance with industry recommendations, a doctor can interpret the results and inform you if your bone density is normal or below average.
Osteopenia, or decreased bone mass, is a diagnosis that doctors make occasionally. Osteoporosis is not present yet. It indicates that the density of your bones is not as high as it may be.
What consequences might osteoporosis cause?

Osteoporosis can raise the risk of bone fractures, especially hip, spine, and wrist fractures.
The International Osteoporosis Foundation estimates that one in three women and one in five men over 50 may break their hips due to osteoporosis worldwide.
Because spinal fractures can shorten the spinal column, they can have the effect of making a person appear shorter. Surgery may be necessary for certain types of bone fractures.
In light of studiesAccording to a reliable source, bone fractures raise your chance of becoming disabled or dying. Specifically, hip fractures are linked to a 15–20% rise in mortality within a year, particularly in men.
In addition to causing bone discomfort, osteoporosis can also impair your capacity to carry out regular tasks.
How is osteoporosis treated?

Osteoporosis treatment involves taking drugs that promote bone growth. These drugs frequently have hormonal effects that stimulate the body’s production of bone by functioning as estrogen substitutes. The following are some examples of drugs used to treat osteoporosis:
- Bisphosphonates
- Calcitonin
- estrogen
- PTH parathyroid hormone (teriparatide)
- proteins connected to parathyroid hormone, like abaloparatide
- Evista, or raloxifene
In April 2019, the FDA approved a more recent drug called romosozumab (Evenity) to treat osteoporosis in women who have gone through menopause and are at high risk of breaking bones.
Due to the medication’s potential to raise the risk of heart attacks or strokes, it comes with a boxed warning. For those who have a history of these diseases, it is not advised.
One surgical procedure for treating fractures is kyphoplasty. By making tiny incisions, a little balloon is inserted into the collapsed vertebrae during a kyphoplasty procedure to give the spine its natural height and functionality back. Cement is used in place of the balloon to restore the bone’s strength.
How can osteoporosis be avoided?
In order to preserve bone density and stop bone loss, action must be taken.
Here are some examples of actions you can take to strengthen your bones:
Take up physical activity

Frequent weightlifting activities promote bone growth. Exercise that requires weight bearing is standing up and using your bones to sustain your body weight. As examples, consider:
- walking
- jogging
- using an elliptical machine
- dancing
- climbing stairs
Consume adequate calcium
The National Institutes of Health state that an adult normally need 1,000 milligrams (mg) of calcium each day. But depending on your demands for calcium and your stage of life, this can change.
Among the foods high in calcium are:
- dairy products with reduced fat content
- tinned salmon and sardines (bones)
- broccoli
- beans or legumes
- greens with collards
- kale
- bok choy
- foods fortified with nutrients, such cereal, bread, and almond milk
See a healthcare practitioner for further details regarding your individual calcium requirements.
Make sure you have enough vitamin D
Take vitamin D every day. Your body needs vitamin D to properly absorb calcium. The average person need 400 international units (IU) of vitamin D daily.
Sunlight exposure for ten to fifteen minutes can increase the production of vitamin D. According to the Skin Cancer Foundation, you can get all the vitamin D you need by wearing sunscreen and spending this little time outside in the sun two or three times a week.
Vitamin D is also found in foods including salmon, egg yolks, and fortified milk.
Avoid falls
One way to lessen the risk of falling indoors is to:
- putting on socks and nonslip shoes
- putting electrical lines up to the walls’ borders
- maintaining light in the rooms
- ensuring that carpets are secured to the ground with tacks
- putting a flashlight at your bedside
- installation of grab bars in the restroom
- clearing clutter from the places you walk
Among the methods to lessen the risk of falling outside are:
- use aids such as a walker or cane
- wearing shoes with friction and rubber soles
- strolling on the lawn when the pavement is wet
- covering ice surfaces with cat litter or salt
Another beneficial preventive measure is to wear the appropriate prescription glasses if you have impaired eyesight.
When walking about your house or outside, there are several exercises that might aid with grip strength and balance. A physical therapist can assist you in designing a customized balance training program, so think about scheduling an appointment with them.
Stay away from harmful chemicals
Osteoporosis risk factors include smoking and substance use disorders, such as alcohol abuse.
You can get resources and support if you’re in need. For instance, if you smoke, see your doctor about the best approach to stop, any helpful smoking aids, or other available options.
When to visit a physician?

Symptoms of osteoporosis can be uncomfortable and painful. If you are in excruciating pain, especially in your wrist, neck, hips, or back, you should schedule an appointment with a doctor very once. It’s possible that you have a fractured bone that needs to be assessed and treated.
Use the Healthline FindCare tool to look up doctors in your region if you need assistance finding a primary care physician.
The bottom line
Your bones will become thinner and more fragile if you have osteoporosis. Osteoporosis is far more common in elderly persons because the body’s capacity to create new bone slows down with age. Men can develop osteoporosis as well, despite the condition primarily affecting women.
Usually, osteoporosis is asymptomatic. It’s possible that you won’t become aware of this illness until you break a bone. Some symptoms, though, such receding gums, weakened grip, and more brittle fingernails, might be early warning indicators.
The most typical signs of later-stage osteoporosis are frequently bone fractures, stooped posture, loss of height, and back or neck pain.
Make sure you schedule an appointment with your physician if you experience any of these symptoms. With the aid of specific tests, they can identify osteoporosis and design a personalized treatment strategy for you.
