Lymphoma represents a diverse group of cancers that originate in the lymphatic system, a vital part of the body’s immune system. This complex disease affects lymphocytes, a type of white blood cell crucial for fighting infections. Lymphoma can arise in lymph nodes throughout the body, as well as in other lymphoid tissues such as the spleen and bone marrow.
Understanding lymphoma involves recognizing its two main categories: Hodgkin lymphoma and non-Hodgkin lymphoma (NHL). Each category comprises numerous subtypes, each with distinct characteristics in terms of cell type, behavior, and treatment approaches.
Lymphoma can present a range of symptoms, including swollen lymph nodes, fever, night sweats, fatigue, and unexplained weight loss. Diagnosis typically involves a combination of imaging studies, blood tests, and biopsy to identify specific characteristics of the cancer cells.
Treatment options for lymphoma depend on the subtype, stage of the disease, and individual patient factors. These may include chemotherapy, radiation therapy, immunotherapy, targeted therapy, and stem cell transplantation.
Advances in research and treatment continue to improve outcomes for individuals diagnosed with lymphoma, highlighting the importance of early detection, personalized treatment plans, and ongoing supportive care.
Table of Contents
Types of Lymphoma
Lymphoma is a diverse group of cancers that originate in the lymphatic system, affecting lymphocytes, a type of white blood cell crucial for immune function. There are two main categories of lymphoma: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). Each category encompasses various subtypes, distinguished by their unique characteristics and behaviors:
1. Hodgkin Lymphoma (HL)
- Classical Hodgkin Lymphoma (cHL):
- Nodular Sclerosis HL: Most common subtype, often affecting young adults, characterized by nodules within lymph nodes.
- Mixed Cellularity HL: More common in older adults, marked by mixed types of cells in affected lymph nodes.
- Lymphocyte-rich HL: Less common, often found in lymph nodes with abundant lymphocytes.
- Lymphocyte-depleted HL: Rare and aggressive form, typically diagnosed at advanced stages.
- Nodular Lymphocyte-Predominant Hodgkin Lymphoma (NLPHL):
- Distinctive subtype characterized by large, popcorn-shaped cells called lymphocyte-predominant cells. Generally has a better prognosis than classical HL.
2. Non-Hodgkin Lymphoma (NHL)
Non-Hodgkin lymphoma encompasses a large and diverse group of lymphomas, including over 60 subtypes. Some common types include:
- B-cell Lymphomas:
- Diffuse Large B-cell Lymphoma (DLBCL): Most common NHL subtype, aggressive in nature but potentially curable with treatment.
- Follicular Lymphoma: Slow-growing NHL that often relapses despite treatment but can be managed effectively for long periods.
- Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (CLL/SLL): Related disorders involving mature B-cells, with CLL primarily affecting the blood and bone marrow, and SLL primarily involving lymph nodes.
- T-cell Lymphomas:
- Peripheral T-cell Lymphoma: Includes several subtypes, often aggressive and challenging to treat due to their rarity and varied presentation.
- Cutaneous T-cell Lymphoma: Affecting the skin primarily, including mycosis fungoides and Sézary syndrome.
- Other Rare Types:
- MALT (Mucosa-Associated Lymphoid Tissue) Lymphoma: Arises from lymphoid tissue in organs such as the stomach, lungs, or thyroid.
- Burkitt Lymphoma: Fast-growing NHL more common in children and characterized by MYC gene abnormalities.
- Primary Mediastinal B-cell Lymphoma: Rare and aggressive NHL originating in the thymus or mediastinal lymph nodes.
Each subtype of lymphoma has distinct clinical features, behaviors, and treatment approaches. Accurate diagnosis and classification are essential for determining the most appropriate treatment and achieving optimal outcomes for patients. Ongoing research and clinical trials continue to advance our understanding and treatment options for these complex diseases.
Symptoms of Lymphoma

The symptoms of lymphoma can vary depending on the type of lymphoma and where it is located in the body. Here are some common symptoms associated with lymphoma:
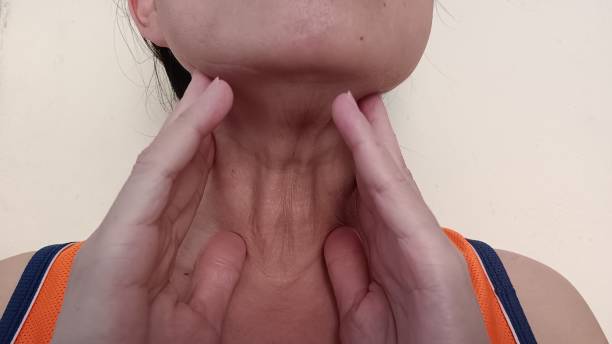
- Swollen Lymph Nodes: The most common symptom of lymphoma is swelling of one or more lymph nodes, usually in the neck, armpit, or groin. These lymph nodes are often painless but may be tender to the touch.
- Fatigue: Persistent tiredness or lack of energy that doesn’t improve with rest.
- Fever: Unexplained fevers that may come and go, often accompanied by chills.
- Night Sweats: Profuse sweating, particularly at night, that may soak through clothing and bedding.
- Unexplained Weight Loss: Significant and unintentional weight loss, typically more than 10% of body weight over 6 months.
- Itching: Generalized itching (pruritus) without an obvious cause.
- Persistent Cough or Chest Pain: Symptoms may occur if lymphoma affects the lymph nodes in the chest or mediastinum.
- Abdominal Symptoms: These may include pain, swelling, or feeling fullness after eating only a small amount (early satiety), particularly if lymphoma involves abdominal lymph nodes or organs.
- Skin Changes: Some lymphomas can cause rash-like skin changes, itching, or lesions.
- Other Symptoms: Depending on the type and location of lymphoma, symptoms may also include bone pain, neurological symptoms (if lymphoma affects the brain or spinal cord), and difficulty breathing (if lymphoma affects the chest or lungs).
It’s important to note that these symptoms can also be caused by conditions other than lymphoma. If you experience persistent symptoms or any concerning changes in your health, it’s advisable to consult with a healthcare provider for proper evaluation and diagnosis. Early detection and treatment can significantly improve outcomes for individuals with lymphoma.
Causes of Lymphoma

The exact causes of lymphoma are not fully understood, but several factors may contribute to its development:
- Genetic Predisposition: Some genetic mutations or inherited conditions may increase the risk of developing lymphoma. However, most cases of lymphoma do not have a clear genetic link.
- Immune System Weakness: Conditions that weaken the immune system, such as HIV/AIDS, organ transplantation (and subsequent immunosuppressive therapy), autoimmune diseases, or certain infections (e.g., Epstein-Barr virus), can increase the risk of lymphoma.
- Age: Lymphomas are more common in older adults, though some types can occur in younger individuals.
- Exposure to Certain Chemicals or Radiation: Prolonged exposure to chemicals like pesticides, solvents, or certain medications (e.g., chemotherapy drugs used for other cancers) may increase the risk. Radiation exposure, such as from previous cancer treatments or environmental sources, is also a known risk factor.
- Infections: Chronic infections with certain viruses, bacteria, or parasites have been associated with an increased risk of lymphoma. For example, Epstein-Barr virus (EBV) is linked to some types of lymphoma, including Burkitt lymphoma and Hodgkin lymphoma.
- Autoimmune Diseases: Some autoimmune conditions, where the immune system mistakenly attacks the body’s own tissues, may slightly increase the risk of certain types of lymphoma.
It’s important to note that while these factors may contribute to the development of lymphoma, many people diagnosed with lymphoma do not have any known risk factors. Research into the causes of lymphoma continues to advance, aiming to better understand and potentially prevent this complex group of cancers.
Risk Factors
Several factors can increase the risk of developing lymphoma. These risk factors vary depending on the type of lymphoma and individual circumstances. Here are some common risk factors associated with lymphoma:
- Age: Lymphoma can occur at any age, but the risk increases with age, especially after 60 years old.
- Gender: Some types of lymphoma are more common in males (e.g., Hodgkin lymphoma), while others have a higher incidence in females (e.g., certain subtypes of non-Hodgkin lymphoma).
- Family History: Having a first-degree relative (parent, sibling, or child) with lymphoma may slightly increase the risk, suggesting a possible genetic predisposition.
- Weakened Immune System: Conditions that weaken the immune system, such as HIV/AIDS, organ transplantation (and subsequent immunosuppressive therapy), autoimmune diseases, or chronic infections, can elevate the risk of lymphoma.
- Infections: Chronic infections with certain viruses, bacteria, or parasites have been linked to an increased risk of lymphoma. For example, Epstein-Barr virus (EBV) is associated with Hodgkin lymphoma and some types of non-Hodgkin lymphoma.
- Previous Cancer Treatment: Radiation therapy or chemotherapy used to treat previous cancers may increase the risk of developing lymphoma later in life.
- Chemical Exposure: Prolonged exposure to certain chemicals, such as pesticides, solvents, or industrial chemicals, has been associated with an increased risk of lymphoma.
- Autoimmune Diseases: Some autoimmune conditions, such as rheumatoid arthritis, systemic lupus erythematosus (SLE), or Sjögren’s syndrome, may slightly increase the risk of certain types of lymphoma.
- Obesity: Obesity has been identified as a potential risk factor for certain types of lymphoma, although the exact mechanisms are not fully understood.
- Personal History: Individuals who have had one type of lymphoma may have a slightly higher risk of developing another type of lymphoma later in life.
It’s important to note that having one or more risk factors does not mean that a person will definitely develop lymphoma. Many people diagnosed with lymphoma do not have any known risk factors, and the presence of risk factors does not necessarily indicate causation. Regular medical check-ups and discussions with healthcare providers can help assess individual risk factors and manage overall health effectively.
Diagnosis

Diagnosing lymphoma involves a series of tests and evaluations to accurately identify the type and extent of the disease. Here are the primary steps and methods used in the diagnosis of lymphoma:
1. Medical History and Physical Examination
- History: The doctor will take a detailed medical history, including any symptoms, risk factors, and family history of lymphoma or other cancers.
- Physical Exam: A thorough physical examination will be conducted, focusing on checking for swollen lymph nodes, spleen, or liver.
2. Laboratory Tests
- Blood Tests: Blood tests can help assess overall health, detect signs of infection, anemia, or other abnormalities. Specific tests include:
- Complete Blood Count (CBC): Measures the levels of different types of blood cells.
- Lactate Dehydrogenase (LDH): Elevated levels can indicate tissue damage and are often higher in lymphoma.
- Erythrocyte Sedimentation Rate (ESR): Higher levels can suggest inflammation or cancer.
3. Imaging Studies
- Chest X-ray: Can detect swollen lymph nodes or other abnormalities in the chest.
- Computed Tomography (CT) Scan: Provides detailed cross-sectional images of the body, helping to identify the size and location of lymph nodes and other affected areas.
- Magnetic Resonance Imaging (MRI): Particularly useful for assessing the brain, spinal cord, or other soft tissues.
- Positron Emission Tomography (PET) Scan: Often combined with a CT scan (PET/CT), this imaging helps detect areas of active lymphoma throughout the body.
4. Lymph Node Biopsy
- Excisional or Incisional Biopsy: The most definitive method of diagnosis. Involves removing an entire lymph node (excisional) or a part of it (incisional) for microscopic examination.
- Core Needle Biopsy: Uses a larger needle to remove a core of tissue from a lymph node.
- Fine Needle Aspiration (FNA) Biopsy: Uses a thin needle to extract a small sample of cells from a lymph node.
5. Bone Marrow Aspiration and Biopsy
- Purpose: Checks for the presence of lymphoma cells in the bone marrow.
- Procedure: Involves taking a small sample of bone marrow tissue and fluid, usually from the hip bone, for microscopic examination.
6. Molecular and Genetic Tests
- Flow Cytometry: Analyzes the types and characteristics of cells in a biopsy sample to distinguish lymphoma from other conditions.
- Immunohistochemistry: Uses antibodies to detect specific proteins on the surface of cells, helping to identify lymphoma subtypes.
- Cytogenetic Analysis: Examines the chromosomes of lymphoma cells for abnormalities.
- Polymerase Chain Reaction (PCR): Detects specific genetic mutations or rearrangements associated with certain types of lymphoma.
7. Staging
- Purpose: Determines the extent and spread of lymphoma, crucial for planning treatment.
- Methods: Combines results from physical exams, imaging studies, and biopsies to assign a stage (I-IV) based on the location and number of affected lymph nodes or organs.
8. Additional Tests
- Lumbar Puncture (Spinal Tap): May be performed if there’s a suspicion that lymphoma has spread to the central nervous system (CNS).
- Ultrasound: Used to examine specific areas like the abdomen or pelvis for enlarged lymph nodes or organ involvement.
Accurate diagnosis and staging of lymphoma are critical for developing an effective treatment plan. If you have symptoms suggestive of lymphoma or if lymphoma is suspected, your healthcare provider will guide you through the appropriate tests and evaluations to confirm the diagnosis and determine the best course of action.
Treatment

The treatment of lymphoma depends on the type, stage, and specific characteristics of the disease, as well as the patient’s overall health and preferences. Here are the primary treatment options for lymphoma:
1. Chemotherapy
- Purpose: Uses drugs to kill cancer cells or stop their growth.
- Administration: Can be given orally, intravenously, or intrathecally (into the cerebrospinal fluid).
- Regimens: Often involves combinations of drugs administered in cycles over several months. Common regimens include CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) for non-Hodgkin lymphoma and ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) for Hodgkin lymphoma.
2. Radiation Therapy
- Purpose: Uses high-energy radiation to kill cancer cells or shrink tumors.
- Types:
- External Beam Radiation: Delivered from outside the body, targeting specific areas affected by lymphoma.
- Internal Radiation: Rarely used for lymphoma, involves placing radioactive material inside the body near cancer cells.
- Usage: Often combined with chemotherapy, especially for localized disease.
3. Targeted Therapy
- Purpose: Uses drugs or other substances to specifically target cancer cells with minimal harm to normal cells.
- Examples:
- Rituximab: A monoclonal antibody targeting CD20 on B-cell lymphomas.
- Brentuximab Vedotin: Targets CD30 on Hodgkin lymphoma cells.
- Ibrutinib: Inhibits Bruton’s tyrosine kinase (BTK) for certain B-cell lymphomas.
- Administration: Usually given intravenously or orally.
4. Immunotherapy
- Purpose: Boosts the body’s natural defenses to fight cancer.
- Types:
- Checkpoint Inhibitors: Drugs like pembrolizumab and nivolumab that help the immune system recognize and attack cancer cells.
- CAR T-cell Therapy: Involves modifying a patient’s T-cells to recognize and kill lymphoma cells.
- Usage: Often for relapsed or refractory lymphoma.
5. Stem Cell Transplantation
- Purpose: Replaces damaged or destroyed bone marrow with healthy stem cells.
- Types:
- Autologous Transplant: Uses the patient’s own stem cells.
- Allogeneic Transplant: Uses stem cells from a donor.
- Procedure: Typically follows high-dose chemotherapy or radiation to eradicate the cancer.
6. Surgery
- Usage: Rarely used as a primary treatment for lymphoma. May be employed to remove a single affected lymph node or mass, or for diagnostic purposes.
7. Watchful Waiting
- Purpose: Monitoring the disease closely without active treatment.
- Usage: For certain slow-growing (indolent) lymphomas that are not causing symptoms or affecting organ function.
8. Clinical Trials
- Purpose: Provides access to new and experimental treatments that are not yet widely available.
- Participation: Patients may consider clinical trials as an option to receive cutting-edge therapies.
9. Supportive Care
- Purpose: Manages symptoms and improves quality of life during and after treatment.
- Types:
- Medications: For pain, nausea, infections, etc.
- Lifestyle Modifications: Nutrition, exercise, and stress management.
- Palliative Care: Comprehensive care to relieve symptoms and improve well-being.
Developing a Treatment Plan
The choice of treatment depends on:
- Type and Stage of Lymphoma: Different types and stages of lymphoma respond to different treatments.
- Patient’s Overall Health: Age, comorbidities, and overall fitness impact treatment choices.
- Side Effects: Potential side effects and their impact on quality of life are considered.
- Patient Preferences: Informed decisions based on understanding the risks and benefits of each treatment option.
Monitoring and Follow-up
Regular follow-up is essential to:
- Assess Treatment Response: Through imaging studies, blood tests, and physical exams.
- Manage Side Effects: Timely intervention for any adverse effects of treatment.
- Detect Recurrence: Early identification of any signs of lymphoma returning.
The management of lymphoma is complex and requires a multidisciplinary approach, involving oncologists, hematologists, radiologists, and supportive care specialists to provide comprehensive care tailored to each patient’s needs.
Prevention

While there is no guaranteed way to prevent lymphoma, certain measures can reduce the risk of developing this type of cancer. Here are some strategies and lifestyle changes that may help lower the risk:
1. Maintain a Healthy Lifestyle
- Balanced Diet: Eat a diet rich in fruits, vegetables, whole grains, and lean proteins. Limit consumption of processed foods, red meats, and foods high in sugar and fat.
- Regular Exercise: Engage in regular physical activity to maintain a healthy weight and boost the immune system.
- Avoid Tobacco: Do not smoke, and avoid exposure to secondhand smoke, as tobacco use is linked to various cancers.
2. Limit Exposure to Infections
- Safe Practices: Use protective measures such as condoms to reduce the risk of infections like HIV and hepatitis C, which are associated with a higher risk of lymphoma.
- Vaccinations: Stay up-to-date with vaccinations, such as the hepatitis B vaccine, which can help prevent infections linked to lymphoma.
- Good Hygiene: Practice good hygiene to reduce the risk of infections that could weaken the immune system.
3. Avoid Harmful Chemicals
- Pesticides and Solvents: Limit exposure to chemicals and pesticides known to increase cancer risk. Use protective equipment if you must handle such substances.
- Occupational Safety: Follow safety guidelines and regulations in the workplace to reduce exposure to hazardous chemicals and radiation.
4. Manage Medical Conditions
- Autoimmune Diseases: If you have an autoimmune disease, work with your healthcare provider to manage it effectively, as some autoimmune conditions are linked to an increased risk of lymphoma.
- Regular Check-ups: Attend regular medical check-ups to monitor and manage chronic health conditions that may increase lymphoma risk.
5. Monitor and Manage Immune System Health
- Immunosuppressive Therapy: If you need immunosuppressive medications (e.g., after an organ transplant), follow your doctor’s guidance to balance the need for these drugs with potential risks.
- Healthy Practices: Engage in practices that support a healthy immune system, such as stress management, adequate sleep, and avoiding excessive alcohol consumption.
6. Reduce Radiation Exposure
- Medical Imaging: Limit exposure to unnecessary medical imaging that uses radiation (e.g., X-rays and CT scans). Only undergo these tests when medically necessary.
- Environmental Factors: Be aware of and limit exposure to environmental sources of radiation.
7. Genetic Counseling and Testing
- Family History: If you have a family history of lymphoma or related cancers, consider genetic counseling. Genetic testing can help assess your risk and guide preventive strategies.
8. Awareness and Early Detection
- Know the Symptoms: Be aware of the common symptoms of lymphoma, such as swollen lymph nodes, unexplained weight loss, and persistent fatigue. Early detection can improve outcomes.
- Regular Screenings: Discuss with your healthcare provider whether you need regular screenings, especially if you have risk factors for lymphoma.
9. Participate in Clinical Research
- Clinical Trials: Consider participating in clinical trials focused on cancer prevention and early detection. Research studies help improve understanding and development of effective preventive measures.
While it’s not always possible to prevent lymphoma, adopting these strategies can help reduce your risk and promote overall health. Regular communication with your healthcare provider is essential to tailor prevention strategies to your individual risk factors and health status.
Living With Lymphoma
Living with lymphoma involves managing the physical, emotional, and practical aspects of the disease and its treatment. Here are key considerations and strategies to help navigate life with lymphoma:
1. Medical Management
- Follow Treatment Plans: Adhere to the treatment regimen prescribed by your healthcare team, which may include chemotherapy, radiation, targeted therapy, or immunotherapy.
- Regular Check-ups: Attend all scheduled appointments for monitoring treatment response, managing side effects, and detecting any recurrence.
- Medication Management: Take prescribed medications as directed and report any side effects to your healthcare provider for timely intervention.
2. Symptom Management
- Manage Side Effects: Work with your healthcare team to manage side effects of treatment, such as fatigue, nausea, pain, and infections.
- Pain Management: Use prescribed pain relief methods and report persistent pain to your healthcare provider.
- Fatigue: Balance activity with rest, and consider light exercise, such as walking, to improve energy levels.
3. Healthy Lifestyle Choices
- Nutrition: Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to support overall health and recovery.
- Physical Activity: Engage in regular physical activity, as tolerated, to maintain strength and improve mood.
- Avoid Infections: Practice good hygiene, avoid close contact with sick individuals, and follow your healthcare provider’s advice on vaccinations and preventive measures.
4. Emotional and Mental Health
- Counseling and Support Groups: Seek support from counselors, psychologists, or support groups for emotional and psychological support.
- Stress Management: Practice stress-reducing techniques such as mindfulness, meditation, yoga, or deep breathing exercises.
- Stay Connected: Maintain connections with family and friends for emotional support and to avoid feelings of isolation.
5. Practical Considerations
- Financial Assistance: Explore options for financial support, including insurance, patient assistance programs, and non-profit organizations that offer financial aid for medical expenses.
- Work and Career: Communicate with your employer about your diagnosis and treatment. Discuss possible adjustments or accommodations, such as flexible hours or working from home.
- Legal Matters: Consider legal guidance for issues such as healthcare proxies, living wills, and disability benefits.
6. Education and Advocacy
- Learn About Your Condition: Educate yourself about lymphoma, its treatment options, and potential side effects. Reliable sources include your healthcare team, cancer organizations, and reputable online resources.
- Advocate for Your Care: Be an active participant in your care. Ask questions, seek second opinions if necessary, and ensure you understand your treatment options and plan.
7. Long-Term Monitoring
- Survivorship Care Plan: After completing treatment, work with your healthcare provider to develop a survivorship care plan that includes regular follow-up visits, screening for recurrence, and monitoring for long-term side effects.
- Healthy Living: Continue to follow a healthy lifestyle to support your long-term health and well-being.
8. Support Networks
- Family and Friends: Lean on your family and friends for emotional, practical, and sometimes financial support.
- Community Resources: Utilize resources from cancer support organizations, community groups, and online forums for additional support and information.
Living with lymphoma is challenging, but with comprehensive medical care, emotional support, and practical planning, many individuals manage to live fulfilling lives during and after treatment. Regular communication with your healthcare team and support network is crucial for addressing the multifaceted aspects of living with lymphoma.
Conclusion
Lymphoma is a complex and varied group of cancers affecting the lymphatic system, with distinct types, symptoms, and causes. The journey from diagnosis to treatment and beyond involves multiple stages, including understanding risk factors, undergoing appropriate diagnostic tests, and receiving targeted therapies tailored to the specific type and stage of lymphoma.
Advancements in medical research have significantly improved the prognosis for many individuals with lymphoma, offering a range of treatment options such as chemotherapy, radiation, targeted therapy, immunotherapy, and stem cell transplantation. These treatments aim to manage the disease effectively, improve survival rates, and enhance the quality of life for patients.
Living with lymphoma requires a comprehensive approach that includes medical management, lifestyle adjustments, emotional and psychological support, and practical considerations. It is crucial for patients to stay informed, actively participate in their care, and seek support from healthcare providers, family, friends, and support networks.
While prevention remains challenging due to the unclear causes of lymphoma, adopting a healthy lifestyle and being vigilant about potential risk factors can contribute to overall well-being and potentially reduce the risk of developing the disease.
Ultimately, with early detection, effective treatment, and holistic support, many individuals with lymphoma can achieve positive outcomes and lead fulfilling lives. Continuous research and advancements in the field of oncology hold promise for even better treatment options and outcomes in the future.
