Herpes is a common viral infection caused by the herpes simplex virus (HSV), affecting millions of people worldwide. There are two primary types of herpes simplex virus: HSV-1, which typically causes oral herpes, and HSV-2, which usually leads to genital herpes. Both types of herpes are highly contagious and can cause recurrent and often painful sores or blisters in the infected area. Despite its prevalence, herpes remains surrounded by misconceptions and stigma, making education and awareness crucial.
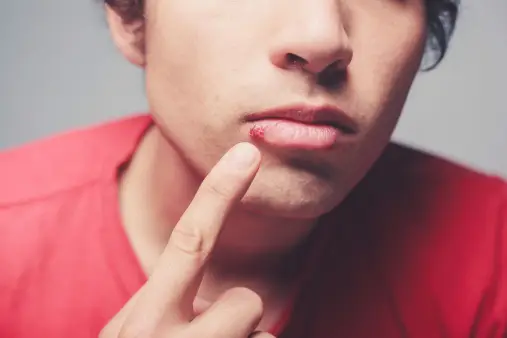
Oral herpes, caused by HSV-1, commonly manifests as cold sores or fever blisters around the mouth and lips. It is primarily transmitted through direct contact with infected saliva or skin, often during childhood. Genital herpes, caused by HSV-2, is a sexually transmitted infection (STI) that affects the genital and anal regions. It spreads through sexual contact with an infected person, even when they may not have visible symptoms.
While there is no cure for herpes, effective treatments are available to manage outbreaks, reduce symptoms, and minimize the risk of transmission. Antiviral medications can help shorten the duration of outbreaks and suppress the virus, making living with herpes more manageable. Understanding the modes of transmission, recognizing the symptoms, and adopting preventive measures are key to controlling the spread of herpes and reducing its impact on individuals’ lives.
This introduction explores the types of herpes, their symptoms, transmission methods, and available treatments, emphasizing the importance of awareness and proactive management in dealing with this widespread infection.
Table of Contents
Types of Herpes

Herpes is primarily caused by two types of herpes simplex viruses: HSV-1 and HSV-2. These viruses are distinct but closely related, each typically responsible for different types of infections. Understanding the differences between these types is essential for proper diagnosis and management.
- Herpes Simplex Virus Type 1 (HSV-1):
- Oral Herpes: HSV-1 is most commonly associated with oral herpes, which causes cold sores or fever blisters around the mouth and lips.
- Transmission: It spreads primarily through direct contact with infected saliva or skin, such as through kissing, sharing eating utensils, or oral-genital contact.
- Symptoms: Initial infection may include fever, sore throat, and swollen lymph nodes, followed by painful blisters or sores on the lips or around the mouth. Recurrent outbreaks are usually milder and can be triggered by stress, illness, or sun exposure.
- Other Infections: HSV-1 can also cause herpetic whitlow (finger infection), herpes gladiatorum (skin infection in athletes), and in rare cases, encephalitis (brain infection).
- Herpes Simplex Virus Type 2 (HSV-2):
- Genital Herpes: HSV-2 is most commonly associated with genital herpes, which affects the genital and anal regions.
- Transmission: It spreads primarily through sexual contact with an infected person, including vaginal, anal, and oral sex. HSV-2 can be transmitted even when there are no visible symptoms.
- Symptoms: Initial infection may include flu-like symptoms such as fever, body aches, and swollen lymph nodes, followed by painful blisters or sores on the genitals, anus, thighs, or buttocks. Recurrent outbreaks are usually less severe and may be preceded by tingling or itching in the affected area.
- Other Infections: HSV-2 can also cause neonatal herpes, a serious infection in newborns contracted during childbirth from an infected mother.
Less Common Types of Herpes Infections
- Herpes Zoster (Shingles):
- Cause: Herpes zoster is caused by the varicella-zoster virus, which also causes chickenpox. It is not caused by HSV-1 or HSV-2 but is part of the herpes virus family.
- Symptoms: Painful rash and blisters that usually occur in a single stripe on one side of the body or face. Shingles can cause long-term nerve pain known as postherpetic neuralgia.
- Transmission: Shingles is not transmitted from person to person, but the varicella-zoster virus can cause chickenpox in someone who has never had it if they come into contact with the fluid from shingles blisters.
Transmission and Prevention
- Transmission: Both HSV-1 and HSV-2 are highly contagious and can be transmitted through direct contact with infected skin, mucous membranes, or bodily fluids. Asymptomatic shedding, where the virus is present on the skin without visible symptoms, also contributes to transmission.
- Prevention: Preventive measures include avoiding direct contact with infected areas, using barrier protection (such as condoms) during sexual activity, and taking antiviral medications to reduce the risk of transmission.
Herpes simplex viruses HSV-1 and HSV-2 are responsible for different types of infections, primarily oral and genital herpes, respectively. Recognizing the differences between these types, understanding their transmission methods, and adopting preventive measures are key to managing herpes infections. With appropriate treatment and awareness, individuals can effectively manage symptoms and reduce the impact of herpes on their lives.
Symptoms of Herpes

Herpes simplex virus (HSV) infections present a range of symptoms, varying in severity and frequency based on the type of virus (HSV-1 or HSV-2) and the site of infection. Here is a detailed look at the symptoms associated with HSV-1 and HSV-2 infections.
Oral Herpes (HSV-1)
- Initial Symptoms:
- Fever: Often accompanies the first outbreak, especially in children.
- Sore Throat: Pain and difficulty swallowing.
- Swollen Lymph Nodes: Particularly in the neck.
- Primary Infection:
- Cold Sores or Fever Blisters: Painful blisters or sores around the mouth and lips.
- Gingivostomatitis: Inflammation of the gums and mouth, which can lead to painful sores inside the mouth.
- Pharyngitis: Inflammation of the pharynx, causing sore throat.
- Recurrent Symptoms:
- Prodromal Symptoms: Tingling, itching, or burning sensation around the lips or mouth before blisters appear.
- Cold Sores: Blisters that eventually burst, crust over, and heal over a period of 1-2 weeks.
- Outbreak Triggers: Stress, illness, sun exposure, and hormonal changes can trigger recurrent outbreaks.
Genital Herpes (HSV-2)
- Initial Symptoms:
- Flu-like Symptoms: Fever, body aches, and swollen lymph nodes.
- Pain: Pain or discomfort in the genital and anal areas.
- Primary Infection:
- Blisters and Sores: Painful blisters or ulcers on the genitals, buttocks, thighs, or anus.
- Urethritis: Inflammation of the urethra, causing pain during urination.
- Vaginal Discharge: Unusual discharge in women.
- Recurrent Symptoms:
- Prodromal Symptoms: Tingling, itching, or pain in the genital area before blisters appear.
- Blisters and Sores: Recurrent blisters that are generally less severe and shorter in duration than the initial outbreak.
- Outbreak Triggers: Stress, illness, fatigue, menstruation, and sexual activity can trigger recurrences.
Less Common Symptoms and Complications
- Herpes Simplex Encephalitis:
- Symptoms: Fever, headache, confusion, seizures, and focal neurological signs.
- Complications: Can lead to severe brain inflammation and requires immediate medical attention.
- Herpetic Whitlow:
- Symptoms: Painful sores or blisters on the fingers or hands.
- Transmission: Often occurs when HSV-1 or HSV-2 is introduced to broken skin on the hands.
- Herpes Gladiatorum:
- Symptoms: Clusters of painful blisters on the face, neck, shoulders, and arms.
- Transmission: Common among athletes who have close skin-to-skin contact.
- Ocular Herpes:
- Symptoms: Pain, redness, swelling, tearing, and sensitivity to light in the eye.
- Complications: Can lead to corneal ulcers and vision loss if untreated.
- Neonatal Herpes:
- Symptoms: Fever, irritability, lethargy, and vesicular lesions on the skin, eyes, or mouth in newborns.
- Transmission: Occurs when a newborn is exposed to HSV during delivery.
Herpes simplex virus infections can present a wide range of symptoms, from mild to severe, depending on the type of virus and site of infection. Early recognition of symptoms and understanding the triggers for recurrent outbreaks are crucial for effective management. If you experience any of these symptoms or suspect a herpes infection, it is important to seek medical advice for diagnosis and appropriate treatment.
Causes of Herpes
Herpes is caused by the herpes simplex virus (HSV), which is divided into two main types: HSV-1 and HSV-2. Understanding the causes and modes of transmission of these viruses is essential for prevention and management.
Herpes Simplex Virus Type 1 (HSV-1)
- Primary Cause:
- HSV-1 is primarily responsible for oral herpes, which manifests as cold sores or fever blisters around the mouth and lips.
- Transmission:
- Direct Contact: HSV-1 is most commonly spread through direct contact with infected saliva, mucous membranes, or skin. This can happen through activities such as kissing, sharing utensils, or touching a cold sore.
- Oral-Genital Contact: HSV-1 can also be transmitted to the genital area through oral-genital contact, leading to genital herpes.
- Risk Factors:
- Age: Primary infection often occurs in childhood.
- Close Contact: Living in close quarters or being in settings where there is frequent skin-to-skin contact increases the risk of transmission.
- Weakened Immune System: Individuals with compromised immune systems are more susceptible to HSV-1 infections and more frequent outbreaks.
Herpes Simplex Virus Type 2 (HSV-2)
- Primary Cause:
- HSV-2 is primarily responsible for genital herpes, which affects the genital and anal regions.
- Transmission:
- Sexual Contact: HSV-2 is predominantly spread through sexual contact, including vaginal, anal, and oral sex. It can be transmitted even when an infected person shows no visible symptoms.
- Mother-to-Newborn: HSV-2 can be transmitted from an infected mother to her baby during childbirth, leading to neonatal herpes.
- Risk Factors:
- Sexual Activity: Having multiple sexual partners or engaging in unprotected sex increases the risk of HSV-2 transmission.
- Previous STIs: A history of other sexually transmitted infections can increase susceptibility to HSV-2.
- Gender: Women are at higher risk of contracting HSV-2 compared to men, partly due to anatomical differences.
Common Factors for Both HSV-1 and HSV-2
- Asymptomatic Shedding:
- Both HSV-1 and HSV-2 can be spread through asymptomatic shedding, where the virus is present on the skin or mucous membranes even in the absence of visible symptoms.
- Trigger Factors for Recurrence:
- Stress: Physical or emotional stress can trigger recurrent outbreaks.
- Illness: Other infections or illnesses can weaken the immune system and precipitate outbreaks.
- Fatigue: Extreme tiredness can lower immune defenses, leading to recurrence.
- Hormonal Changes: Hormonal fluctuations, such as those during menstruation, can trigger outbreaks.
- Sun Exposure: Ultraviolet light exposure can precipitate oral herpes outbreaks.
Prevention Strategies
- Safe Sexual Practices:
- Condom Use: Using condoms can reduce the risk of HSV-2 transmission but may not completely eliminate it, as the virus can be present on skin not covered by a condom.
- Monogamous Relationships: Engaging in mutually monogamous relationships with a partner who has tested negative for HSV reduces the risk.
- Avoiding Direct Contact with Sores:
- Do Not Share Personal Items: Avoid sharing eating utensils, lip balm, or towels with someone who has a cold sore.
- Hand Hygiene: Wash hands thoroughly after touching affected areas to prevent the spread of the virus.
- Reducing Triggers:
- Stress Management: Practices such as yoga, meditation, and regular exercise can help manage stress.
- Healthy Lifestyle: Maintaining a balanced diet, getting adequate sleep, and avoiding excessive sun exposure can reduce the frequency of outbreaks.
- Antiviral Medications:
- Prophylactic Use: Taking antiviral medications on a long-term basis can help prevent recurrent outbreaks and reduce the risk of transmission.
Herpes is caused by the herpes simplex virus, with HSV-1 typically causing oral herpes and HSV-2 causing genital herpes. Understanding the modes of transmission and risk factors for both types of herpes is crucial for prevention and effective management. Safe sexual practices, avoiding direct contact with sores, and managing triggers are key strategies to reduce the spread and impact of herpes infections.
Diagnosis of Herpes

Diagnosing herpes involves a combination of medical history assessment, physical examination, and laboratory tests. Early and accurate diagnosis is crucial for effective management and treatment. Here are the primary methods used in diagnosing herpes simplex virus (HSV) infections:
- Medical History and Physical Examination:
- Symptom Inquiry: The healthcare provider will ask about any symptoms, including the presence of blisters, sores, pain, itching, and any recent potential exposure to the virus.
- Visual Inspection: The provider will visually inspect the affected area for characteristic signs of herpes, such as blisters or sores.
- Laboratory Tests:
- Viral Culture:
- Procedure: A sample is taken from a fresh sore or blister by swabbing the fluid. The sample is then cultured in a laboratory to see if the virus grows.
- Effectiveness: Most effective if done within 48 hours of the appearance of symptoms, but may not always detect the virus if the sores have started to heal.
- Polymerase Chain Reaction (PCR) Test:
- Procedure: PCR testing involves amplifying the genetic material of the virus from a sample taken from sores, blood, or other bodily fluids.
- Effectiveness: Highly sensitive and can differentiate between HSV-1 and HSV-2. It is particularly useful for diagnosing infections of the central nervous system.
- Antibody Tests (Serology):
- Procedure: Blood tests are used to detect antibodies against HSV-1 and HSV-2, indicating a past or current infection.
- Effectiveness: Useful for identifying past infections but may not differentiate between recent and older infections. IgM antibodies indicate recent infection, while IgG antibodies indicate past exposure.
- Direct Fluorescent Antibody (DFA) Test:
- Procedure: A sample from a sore is stained with a fluorescent dye that binds to HSV antigens, which are then viewed under a special microscope.
- Effectiveness: Can quickly identify HSV in the sample but requires specialized equipment.
- Viral Culture:
- Tzanck Smear:
- Procedure: A sample of cells is scraped from a sore and examined under a microscope for characteristic changes caused by herpes.
- Effectiveness: Less commonly used today due to the availability of more accurate tests, but it can provide quick results in some settings.
- Biopsy:
- Procedure: In rare cases, a small piece of tissue from a sore is removed and examined under a microscope.
- Effectiveness: Typically used when the diagnosis is uncertain, and other tests are inconclusive.
Special Considerations
- Genital Herpes:
- Initial Testing: For suspected genital herpes, viral culture and PCR tests are commonly used to confirm the diagnosis.
- Recurrent Testing: Recurrent outbreaks can be confirmed with viral culture or PCR if new sores appear.
- Neonatal Herpes:
- Testing Newborns: PCR and viral culture are crucial for diagnosing herpes in newborns, who can acquire the virus during delivery from an infected mother.
- Herpes Encephalitis:
- Central Nervous System Infections: PCR testing of cerebrospinal fluid (CSF) is the gold standard for diagnosing herpes encephalitis.
Accurate diagnosis of herpes is essential for effective treatment and management. Medical history, physical examination, and a variety of laboratory tests, including viral culture, PCR, and antibody tests, are used to confirm the presence of HSV-1 or HSV-2. Early diagnosis can help in managing symptoms, reducing transmission, and providing appropriate treatment to improve quality of life. If you suspect a herpes infection, seek medical advice for prompt evaluation and testing.
Treatment of Herpes

While there is no cure for herpes simplex virus (HSV) infections, effective treatments are available to manage symptoms, reduce the frequency of outbreaks, and decrease the risk of transmission. Treatment strategies vary depending on whether the infection is primary, recurrent, or chronic. Here are the main approaches to treating herpes:
- Antiviral Medications:
- Acyclovir (Zovirax):
- Use: Widely used for both HSV-1 and HSV-2 infections.
- Administration: Available in oral, topical, and intravenous forms. Oral acyclovir is commonly used for treatment and suppression, while intravenous acyclovir is reserved for severe cases.
- Valacyclovir (Valtrex):
- Use: An oral medication that is converted to acyclovir in the body. It has a longer half-life, allowing for less frequent dosing.
- Administration: Typically used for treating and suppressing both HSV-1 and HSV-2. It is also effective in reducing the risk of transmission.
- Famciclovir (Famvir):
- Use: Another oral antiviral that is effective against HSV-1 and HSV-2.
- Administration: Similar to valacyclovir, it can be used for episodic treatment or chronic suppression.
- Acyclovir (Zovirax):
- Initial Infection Treatment:
- Primary Outbreak: Antiviral medications are most effective when started within the first 72 hours of symptom onset. Treatment usually lasts 7-10 days and helps reduce the severity and duration of the outbreak.
- Pain Management: Over-the-counter pain relievers such as acetaminophen or ibuprofen can help manage pain and discomfort. Topical anesthetics like lidocaine can also provide relief.
- Recurrent Outbreaks:
- Episodic Therapy: Short courses of antiviral medications are taken at the onset of symptoms or during prodromal (early) signs of an outbreak to reduce severity and duration.
- Suppressive Therapy: For individuals with frequent outbreaks (more than six per year), daily antiviral medication can help reduce the frequency and severity of outbreaks. Suppressive therapy also lowers the risk of transmitting the virus to sexual partners.
- Severe and Complicated Cases:
- Intravenous Antivirals: Severe cases, such as herpes encephalitis or neonatal herpes, may require hospitalization and intravenous antiviral therapy.
- Ocular Herpes: HSV infections of the eye (herpes keratitis) are treated with topical antiviral eye drops or ointments, and sometimes oral antivirals, to prevent complications and preserve vision.
- Supportive Care:
- Hydration: Staying well-hydrated helps support the immune system and overall recovery.
- Hygiene: Keeping affected areas clean and dry to prevent secondary infections.
- Comfort Measures: Wearing loose-fitting clothing and using cool compresses can help alleviate discomfort.
- Lifestyle and Home Remedies:
- Stress Management: Techniques such as yoga, meditation, and regular exercise can help manage stress, which may reduce the frequency of outbreaks.
- Healthy Diet: Maintaining a balanced diet rich in vitamins and minerals supports the immune system.
- Avoiding Triggers: Identifying and avoiding personal triggers, such as excessive sun exposure or fatigue, can help prevent outbreaks.
- Prevention and Reducing Transmission:
- Safe Sexual Practices: Using condoms and dental dams during sexual activity reduces the risk of transmission but does not eliminate it completely.
- Disclosure: Communicating with sexual partners about HSV status and taking precautions to reduce transmission.
- Antiviral Prophylaxis: Daily antiviral medication for the infected person can significantly reduce the risk of transmitting HSV to uninfected partners.
While herpes simplex virus infections cannot be cured, effective treatments are available to manage symptoms, reduce outbreak frequency, and minimize transmission risk. Antiviral medications such as acyclovir, valacyclovir, and famciclovir are the mainstay of treatment, providing relief and preventing complications. Supportive care, lifestyle adjustments, and preventive measures further help individuals manage the condition and maintain a good quality of life. If you suspect a herpes infection, seek medical advice for appropriate diagnosis and treatment options tailored to your needs.
Prevention of Herpes
Preventing herpes simplex virus (HSV) infections involves a combination of strategies aimed at reducing the risk of transmission and protecting oneself and others. Here are the key preventive measures:
- Safe Sexual Practices:
- Condom Use: Consistently using condoms during vaginal, anal, and oral sex reduces the risk of HSV transmission. While condoms do not cover all areas that can shed the virus, they significantly lower the risk.
- Dental Dams: Using dental dams during oral sex can help prevent the transmission of HSV.
- Monogamous Relationships: Engaging in mutually monogamous relationships with a partner who has tested negative for HSV reduces the risk.
- Sexual Abstinence During Outbreaks: Avoiding sexual activity during active outbreaks and for a few days after the sores have healed can prevent transmission.
- Communication with Partners:
- Disclosure: Being open with sexual partners about HSV status allows for informed decisions and mutual precautions.
- Joint Prevention Strategies: Partners can work together to reduce transmission risks, including the use of antiviral medications and protective barriers.
- Antiviral Medications:
- Suppressive Therapy: For those with frequent outbreaks or to reduce transmission risk, daily antiviral medications (such as valacyclovir) can be used to lower viral shedding and the likelihood of passing the virus to a partner.
- Episodic Treatment: Taking antiviral medications at the onset of symptoms can reduce the severity and duration of an outbreak, potentially lowering the risk of transmission.
- Avoiding Direct Contact with Sores:
- No Sharing Personal Items: Avoid sharing eating utensils, lip balm, or towels with someone who has an active HSV outbreak.
- Proper Hygiene: Washing hands thoroughly after touching a sore and avoiding touching other parts of the body, especially the eyes and genital area.
- Managing Triggers:
- Stress Reduction: Managing stress through relaxation techniques, regular exercise, and adequate sleep can help prevent outbreaks.
- Healthy Lifestyle: Maintaining a healthy diet and strong immune system can reduce the frequency of outbreaks.
- Sun Protection: Using lip balm with sunblock and avoiding excessive sun exposure can prevent oral herpes outbreaks.
- Maternal Health:
- Pregnant Women: Women with HSV should inform their healthcare providers, as antiviral medication can be prescribed during pregnancy to reduce the risk of transmission to the baby. In some cases, a cesarean delivery may be recommended if active lesions are present at the time of delivery to prevent neonatal herpes.
- Vaccination Research:
- Future Vaccines: Research is ongoing to develop vaccines that could prevent HSV infections. Staying informed about advancements in vaccine development can provide additional preventive options in the future.
Educational and Supportive Measures
- Awareness and Education:
- Understanding Transmission: Educating oneself and partners about how HSV is transmitted and the importance of preventive measures.
- Recognizing Symptoms: Being able to identify early signs of an outbreak to take prompt action and prevent spreading the virus.
- Regular Medical Check-ups:
- Screening: Regular STI screenings can help detect HSV and other sexually transmitted infections early, allowing for timely management and prevention of complications.
- Consultation: Regular consultations with healthcare providers to discuss preventive strategies and manage any outbreaks effectively.
Complications of Herpes
Herpes simplex virus (HSV) infections can lead to various complications, particularly if left untreated or improperly managed. These complications can affect different parts of the body and significantly impact a person’s quality of life. Here are the main complications associated with HSV infections:
- Recurrent Outbreaks:
- Frequency: Some individuals experience frequent and severe recurrent outbreaks, which can be painful and disruptive.
- Impact: Recurrent outbreaks can cause physical discomfort, emotional distress, and affect daily activities and relationships.
- Psychological and Social Impact:
- Stigma and Isolation: The social stigma associated with herpes can lead to feelings of shame, guilt, and isolation.
- Mental Health: Chronic stress, anxiety, and depression are common among individuals with recurrent outbreaks or those struggling with the social implications of the infection.
- Neonatal Herpes:
- Transmission: Pregnant women with active genital herpes can transmit the virus to their baby during childbirth, leading to neonatal herpes.
- Symptoms: Newborns can develop skin, eye, or mouth sores, severe systemic infections, or central nervous system involvement.
- Severity: Neonatal herpes can be life-threatening and requires immediate medical attention.
- Herpes Simplex Encephalitis:
- Cause: HSV can infect the brain, leading to encephalitis, a rare but severe condition.
- Symptoms: Symptoms include fever, headache, confusion, seizures, and focal neurological signs.
- Complications: Herpes encephalitis can cause permanent neurological damage or be fatal if not treated promptly.
- Ocular Herpes (Herpes Keratitis):
- Cause: HSV infection of the eye can lead to herpetic keratitis.
- Symptoms: Symptoms include pain, redness, blurred vision, tearing, and sensitivity to light.
- Complications: If untreated, ocular herpes can cause corneal scarring, vision loss, or blindness.
- Herpetic Whitlow:
- Cause: HSV infection of the fingers, usually through broken skin.
- Symptoms: Painful blisters and sores on the fingers or hands.
- Impact: Herpetic whitlow can be particularly problematic for healthcare workers or individuals who work with their hands.
- Herpes Gladiatorum:
- Cause: HSV infection spread through close skin-to-skin contact, common among athletes.
- Symptoms: Clusters of painful blisters on the face, neck, shoulders, and arms.
- Impact: Can lead to frequent outbreaks and discomfort in affected individuals.
- Systemic Infections in Immunocompromised Individuals:
- Risk: Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are at higher risk for severe and widespread HSV infections.
- Complications: In these individuals, HSV can cause extensive skin lesions, esophagitis, pneumonitis, and disseminated infections.
- Erythema Multiforme:
- Cause: A hypersensitivity reaction that can be triggered by HSV infection.
- Symptoms: Red, target-like lesions on the skin, often accompanied by mucous membrane involvement.
- Severity: In severe cases, it can lead to Stevens-Johnson syndrome or toxic epidermal necrolysis, which are medical emergencies.
- Urinary and Fecal Incontinence:
- Cause: Severe genital herpes can cause inflammation around the sacral nerves, leading to temporary incontinence.
- Symptoms: Difficulty controlling urination or bowel movements.
Herpes simplex virus infections can lead to various complications, ranging from frequent recurrent outbreaks to severe systemic infections and significant psychological impacts. Early diagnosis, effective management, and awareness of potential complications are crucial for minimizing their impact. Regular medical follow-ups, antiviral treatments, and supportive care play essential roles in managing herpes and preventing serious health issues. If you suspect any complications from herpes, seek immediate medical advice to ensure prompt and appropriate care.
Living With Herpes
Living with herpes simplex virus (HSV) can present a range of physical, emotional, and social challenges. However, with effective management strategies and support, individuals can lead healthy and fulfilling lives. Here are key aspects to consider for living well with herpes:
- Medical Management:
- Antiviral Medications: Regular use of antiviral medications like acyclovir, valacyclovir, or famciclovir can help manage outbreaks, reduce symptoms, and decrease the risk of transmission.
- Symptom Relief: Over-the-counter pain relievers, topical anesthetics, and warm baths can alleviate pain and discomfort during outbreaks.
- Regular Check-Ups: Maintain regular appointments with a healthcare provider to monitor the condition, manage symptoms, and address any concerns.
- Lifestyle Adjustments:
- Healthy Diet: Eating a balanced diet rich in vitamins and minerals supports overall health and immune function.
- Exercise: Regular physical activity helps reduce stress and boost the immune system.
- Adequate Rest: Ensuring sufficient sleep helps the body recover and maintain a strong immune system.
- Stress Management: Techniques such as yoga, meditation, deep breathing exercises, and mindfulness can help manage stress, which is a common trigger for outbreaks.
- Managing Outbreaks:
- Recognize Triggers: Identify and avoid personal triggers such as stress, fatigue, illness, and sun exposure.
- Early Intervention: At the first sign of an outbreak (tingling, itching), start antiviral medications to reduce the severity and duration.
- Hygiene: Keep the affected area clean and dry to prevent secondary infections. Avoid touching sores and wash hands frequently.
- Preventing Transmission:
- Safe Sexual Practices: Use condoms and dental dams to reduce the risk of transmission. Avoid sexual contact during outbreaks and for a few days after sores have healed.
- Disclosure: Open and honest communication with sexual partners about HSV status helps manage expectations and take precautions.
- Antiviral Prophylaxis: Daily antiviral medication can reduce the risk of transmitting the virus to an uninfected partner.
- Emotional and Psychological Support:
- Counseling: Professional counseling or therapy can help address the emotional impact of living with herpes, including anxiety, depression, and self-esteem issues.
- Support Groups: Joining support groups provides a community of individuals facing similar challenges, offering mutual support and shared experiences.
- Education: Educating yourself and others about herpes can reduce stigma and promote understanding and acceptance.
- Social and Relationship Considerations:
- Open Communication: Discussing your condition with potential partners can foster trust and mutual respect.
- Support System: Rely on friends, family, and support groups for emotional and practical support.
- Self-Care: Prioritize self-care and mental health by engaging in activities that bring joy and relaxation.
- Special Considerations for Pregnant Women:
- Medical Supervision: Pregnant women with HSV should work closely with their healthcare provider to manage the infection and reduce the risk of neonatal herpes.
- Antiviral Therapy: Antiviral medications may be prescribed during pregnancy to prevent outbreaks and reduce the risk of transmission during delivery.
Living with herpes requires a comprehensive approach that includes medical management, lifestyle adjustments, emotional support, and preventive measures. By taking proactive steps to manage outbreaks, reduce transmission risk, and maintain overall health, individuals with herpes can lead fulfilling lives. Open communication, education, and support from healthcare providers, counselors, and support groups are essential components in effectively managing the condition and overcoming the challenges associated with it.
Conclusion
Living with herpes can be challenging due to the physical, emotional, and social aspects of the condition. However, with effective management strategies and the right support, individuals can lead healthy and fulfilling lives. Understanding the nature of the herpes simplex virus (HSV), recognizing triggers, and promptly addressing outbreaks are key components of managing the condition.
Antiviral medications play a crucial role in controlling symptoms, reducing the frequency of outbreaks, and minimizing the risk of transmission. Additionally, adopting a healthy lifestyle, managing stress, and maintaining good hygiene practices can further help in managing the condition effectively.
Open communication with partners, friends, and healthcare providers is vital for reducing stigma, fostering understanding, and building a supportive network. Emotional and psychological support, whether through counseling or support groups, is essential for coping with the mental health challenges that may arise from living with herpes.
By taking a proactive and informed approach to managing herpes, individuals can navigate the complexities of the condition and maintain a high quality of life. Education, awareness, and support are key elements in overcoming the challenges associated with herpes and ensuring that individuals can live their lives to the fullest despite the condition.
