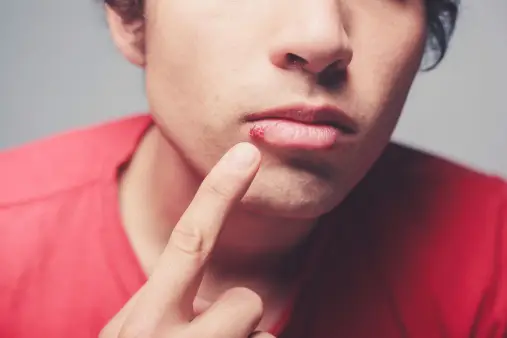
Cold sores, also known as fever blisters, are a common and highly contagious viral infection caused by the herpes simplex virus (HSV). Typically appearing as painful, fluid-filled blisters on or around the lips, cold sores can cause significant discomfort and social distress. These sores usually heal within two to four weeks, but the virus remains dormant in the body, often reactivating and causing recurrent outbreaks.
Understanding the triggers, symptoms, and treatment options for cold sores is crucial for managing and reducing their impact. This introduction aims to provide a comprehensive overview of cold sores, including their causes, transmission, prevention strategies, and effective treatments, offering valuable insights into this widespread and often recurrent condition.
Cold sores, also known as fever blisters, are primarily caused by the herpes simplex virus (HSV). There are two main types of HSV that can cause cold sores, each with distinct characteristics and implications:
Table of Contents
Types of Cold Sores

1. Herpes Simplex Virus Type 1 (HSV-1)
- Prevalence: HSV-1 is the most common cause of cold sores. It is estimated that a significant portion of the global population is infected with HSV-1, often acquired during childhood.
- Symptoms: HSV-1 typically causes cold sores around the lips and mouth, but it can also infect the eyes and, in rare cases, the central nervous system.
- Transmission: The virus is primarily spread through direct contact with an infected person’s saliva or skin, such as kissing or sharing personal items like lip balm or utensils. HSV-1 can also be spread through oral-genital contact, leading to genital herpes.
- Recurrence: HSV-1 remains dormant in nerve cells and can reactivate due to various triggers, such as stress, illness, sunlight, or hormonal changes, leading to recurrent cold sores.
2. Herpes Simplex Virus Type 2 (HSV-2)
- Prevalence: While HSV-2 is more commonly associated with genital herpes, it can also cause cold sores on the lips and mouth, though this is less frequent.
- Symptoms: When HSV-2 causes cold sores, the symptoms are similar to those caused by HSV-1, including painful blisters and sores around the mouth.
- Transmission: HSV-2 is typically transmitted through sexual contact, including oral-genital contact, which can result in oral HSV-2 infections.
- Recurrence: Like HSV-1, HSV-2 can lie dormant in the body and reactivate, causing recurrent outbreaks of cold sores or genital sores.
Cold sores are primarily caused by two types of herpes simplex viruses: HSV-1 and HSV-2. HSV-1 is the most common cause of cold sores around the mouth, while HSV-2, usually associated with genital herpes, can also cause oral infections. Both types of viruses can remain dormant in the body and reactivate under certain conditions, leading to recurrent outbreaks. Understanding the differences between HSV-1 and HSV-2, their transmission routes, and triggers for reactivation is essential for managing and preventing cold sores effectively.
Symptoms of Cold Sores

Cold sores, also known as fever blisters, present a series of recognizable symptoms that progress through distinct stages. Here’s an overview of these symptoms:
Initial Symptoms
- Tingling and Itching:
- The first sign of a cold sore is usually a tingling, itching, or burning sensation around the lips or affected area. This prodromal phase can occur one to two days before the blisters become visible.
Appearance of Blisters
- Small, Fluid-Filled Blisters:
- Clusters of small, painful blisters filled with clear fluid appear on or around the lips, mouth, or nose. These blisters can sometimes form on the gums or the roof of the mouth.
Blister Rupture
- Weeping and Crusting:
- The blisters eventually burst, leaving shallow, open sores that ooze fluid. This stage is highly contagious due to the release of viral particles.
- The open sores then crust over, forming a yellowish-brown scab.
Healing Stage
- Scabbing and Healing:
- The scabs gradually shrink and flake off as the sores heal. The skin may appear slightly pink or red after the scabs fall off.
- Complete healing usually takes two to four weeks without leaving a scar, although in severe cases, mild scarring may occur.
Accompanying Symptoms
In addition to localized symptoms around the affected area, cold sores may be accompanied by systemic symptoms, especially during the initial outbreak:
- Fever:
- A mild to moderate fever can occur, particularly in children and individuals experiencing their first outbreak.
- Swollen Lymph Nodes:
- The lymph nodes near the affected area (e.g., neck or jaw) may become swollen and tender.
- Sore Throat and Difficulty Swallowing:
- Some individuals may experience a sore throat or pain while swallowing, especially if the sores extend into the mouth.
Recurrent Symptoms
Cold sores tend to recur, often in the same location, and the symptoms during recurrent outbreaks are generally milder and shorter in duration compared to the initial outbreak. Common triggers for recurrence include:
- Stress
- Fatigue
- Illness (e.g., cold or flu)
- Sun exposure
- Hormonal changes (e.g., menstruation)
Cold sores progress through distinct stages, starting with tingling and itching, followed by the appearance of blisters, rupture, and crusting, and finally healing. Recognizing these symptoms early can help in managing the condition more effectively. Accompanying symptoms such as fever, swollen lymph nodes, and sore throat may also occur, especially during the first outbreak. Recurrent episodes are common and are usually triggered by factors like stress, illness, or sun exposure. Understanding these symptoms is key to early intervention and reducing the impact of cold sores.
Causes of Cold Sores

Cold sores, also known as fever blisters, are primarily caused by the herpes simplex virus (HSV). There are two types of herpes simplex virus that can cause cold sores: HSV-1 and HSV-2. Understanding the causes of cold sores involves exploring the nature of these viruses, how they spread, and what triggers their reactivation. Here’s a detailed overview:
1. Herpes Simplex Virus Type 1 (HSV-1)
- Primary Cause: HSV-1 is the most common cause of cold sores. It is highly contagious and spreads through direct contact with an infected person’s saliva or skin, such as kissing, sharing utensils, lip balm, or other personal items.
- Primary Infection: The initial infection with HSV-1 often occurs in childhood and can be asymptomatic or cause mild symptoms. After the initial infection, the virus remains dormant in the body’s nerve cells.
- Reactivation: HSV-1 can reactivate and cause recurrent cold sores. The virus travels along the nerves to the skin, where it causes blisters and sores.
2. Herpes Simplex Virus Type 2 (HSV-2)
- Less Common Cause: While HSV-2 is typically associated with genital herpes, it can also cause cold sores around the mouth. This occurs primarily through oral-genital contact.
- Transmission: HSV-2 spreads through sexual contact and can be transmitted even when no sores or symptoms are present.
Triggers for Reactivation
Certain factors can trigger the reactivation of HSV-1 or HSV-2, leading to the development of cold sores:
- Stress:
- Physical or emotional stress can weaken the immune system, making it easier for the virus to reactivate.
- Illness:
- Common illnesses, such as colds or the flu, can trigger an outbreak.
- Sun Exposure:
- Prolonged exposure to sunlight, particularly UV rays, can trigger cold sores in some individuals.
- Fatigue:
- Lack of sleep or extreme tiredness can weaken the immune system and trigger an outbreak.
- Hormonal Changes:
- Hormonal fluctuations, such as those occurring during menstruation, pregnancy, or menopause, can trigger cold sores.
- Injury to the Skin:
- Trauma or injury to the skin around the mouth, including cuts, burns, or cosmetic procedures, can trigger an outbreak.
- Weakened Immune System:
- Conditions or treatments that suppress the immune system, such as HIV/AIDS, chemotherapy, or steroid medications, can lead to frequent or severe outbreaks.
Cold sores are caused primarily by the herpes simplex virus type 1 (HSV-1) and, less commonly, by herpes simplex virus type 2 (HSV-2). These viruses spread through direct contact and can remain dormant in the body’s nerve cells, reactivating in response to various triggers such as stress, illness, sun exposure, fatigue, hormonal changes, skin injury, and weakened immune system. Understanding the causes and triggers of cold sores is crucial for managing and preventing outbreaks effectively.
Diagnosis of Cold Sores
Diagnosing cold sores typically involves a combination of clinical evaluation and, if necessary, laboratory tests. Healthcare providers can often diagnose cold sores based on their characteristic appearance and patient history, but in some cases, additional tests are required to confirm the diagnosis and identify the specific virus responsible. Here’s a detailed overview of the diagnostic process for cold sores:
Clinical Evaluation
- Medical History:
- The healthcare provider will ask about the patient’s symptoms, including the onset, duration, and frequency of the sores. They may also inquire about any known triggers, such as stress, illness, or sun exposure.
- A history of similar sores or previous herpes infections may be discussed.
- Physical Examination:
- The provider will examine the affected area, looking for characteristic signs of cold sores such as clusters of small, fluid-filled blisters on or around the lips, mouth, or nose.
- The presence of a tingling or burning sensation before the appearance of sores may also be a key diagnostic clue.
Laboratory Tests
If the diagnosis is unclear or if it’s necessary to confirm the presence of the herpes simplex virus, the healthcare provider may recommend one or more of the following laboratory tests:
- Viral Culture:
- A sample of fluid from the blister is collected using a swab and sent to a laboratory where the virus can be grown and identified. This test is most effective when performed during the early stages of the blister.
- Polymerase Chain Reaction (PCR) Test:
- This test detects the DNA of the herpes simplex virus in a sample taken from the blister, saliva, or blood. PCR is highly sensitive and can distinguish between HSV-1 and HSV-2.
- Direct Fluorescent Antibody (DFA) Test:
- A sample from the blister is treated with antibodies that bind to the herpes virus and fluoresce under a special microscope. This test helps identify the presence of HSV.
- Blood Tests:
- Blood tests can detect antibodies to HSV-1 and HSV-2, indicating past or current infection. While these tests can confirm exposure to the virus, they are not typically used to diagnose an active outbreak because they do not differentiate between past and current infections.
Differential Diagnosis
It’s important to distinguish cold sores from other conditions that can cause similar symptoms. The healthcare provider may consider the following differential diagnoses:
- Aphthous Ulcers (Canker Sores):
- These are painful ulcers that occur inside the mouth and are not caused by the herpes virus. They lack the characteristic blister phase of cold sores.
- Impetigo:
- A bacterial skin infection that can cause sores around the mouth, often due to Staphylococcus or Streptococcus bacteria.
- Angular Cheilitis:
- Inflammation and cracking at the corners of the mouth, often due to fungal infection, nutritional deficiencies, or irritation.
Diagnosing cold sores involves a combination of medical history, physical examination, and, when necessary, laboratory tests such as viral culture, PCR, DFA, and blood tests. Accurate diagnosis is essential for effective management and treatment, as well as for distinguishing cold sores from other conditions with similar presentations. If you suspect you have cold sores, consulting a healthcare provider for a proper diagnosis and appropriate treatment is recommended.
Treatment

Treating cold sores involves a combination of antiviral medications, topical treatments, and home remedies to alleviate symptoms, speed up healing, and reduce the frequency of outbreaks. Here’s a comprehensive overview of the treatment options for cold sores:
Antiviral Medications
- Oral Antiviral Medications:
- Acyclovir (Zovirax), Valacyclovir (Valtrex), and Famciclovir (Famvir): These prescription medications can help reduce the severity and duration of cold sores if taken at the first sign of an outbreak. They can also be taken daily as suppressive therapy to prevent frequent recurrences.
- Topical Antiviral Creams:
- Acyclovir Cream (Zovirax) and Penciclovir Cream (Denavir): These creams can be applied directly to the cold sores to help speed up healing. They are most effective when used at the earliest signs of tingling or itching.
Over-the-Counter Treatments
- Docosanol (Abreva):
- This over-the-counter cream can shorten the healing time and duration of symptoms if applied at the first sign of an outbreak.
- Analgesic and Antiseptic Creams:
- Creams containing ingredients like benzocaine, lidocaine, or phenol can help reduce pain and discomfort. Antiseptic creams can help prevent secondary bacterial infections.
Home Remedies and Lifestyle Changes
- Cold Compresses:
- Aloe Vera Gel:
- Aloe vera has soothing and anti-inflammatory properties that can help alleviate symptoms and promote healing.
- Honey:
- Applying honey to the cold sore can help with healing due to its antiviral and antibacterial properties.
- Lysine Supplements:
- Some studies suggest that taking lysine supplements may help reduce the frequency of outbreaks and speed up healing.
- Avoiding Triggers:
- Identifying and avoiding triggers such as stress, prolonged sun exposure, and certain foods can help reduce the frequency of outbreaks.
Pain Relief
- Over-the-Counter Pain Relievers:
- Non-prescription pain relievers like ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) can help reduce pain and discomfort associated with cold sores.
Treating cold sores involves a combination of antiviral medications, over-the-counter treatments, home remedies, and preventive measures. Early intervention with antiviral medications can reduce the severity and duration of an outbreak, while topical treatments and home remedies can alleviate symptoms. Preventive strategies, such as avoiding known triggers and maintaining good hygiene, can help reduce the frequency of recurrences. If cold sores are severe or recurrent, consulting a healthcare provider for tailored treatment options is recommended.
Prevention

Preventing cold sores involves a combination of lifestyle modifications, good hygiene practices, and potentially antiviral medications to reduce the risk of outbreaks. Here are effective strategies to help prevent cold sores:
Lifestyle Modifications
- Manage Stress:
- Stress is a common trigger for cold sores. Practice stress management techniques such as meditation, deep breathing exercises, yoga, and regular physical activity.
- Adequate Sleep:
- Ensure you get enough sleep each night to maintain a healthy immune system, which can help prevent outbreaks.
- Healthy Diet:
- Maintain a balanced diet rich in vitamins and minerals, which supports overall immune health. Foods high in lysine and low in arginine may help reduce the frequency of outbreaks.
Sun Protection
- Use Sunscreen:
- Apply a broad-spectrum sunscreen with an SPF of 30 or higher to your lips and face, especially if you plan to be in the sun for extended periods.
- Protective Lip Balm:
- Use a lip balm that contains sunscreen to protect your lips from UV rays, which can trigger cold sores.
Hygiene Practices
- Avoid Sharing Personal Items:
- Do not share items like lip balm, utensils, towels, or razors with others, as these can spread the herpes simplex virus.
- Wash Hands Frequently:
- Regularly wash your hands with soap and water, especially after touching your face or applying medication to a cold sore.
- Avoid Touching Your Face:
- Try not to touch your face or cold sores unnecessarily to prevent spreading the virus to other parts of your body or to other people.
Recognizing and Avoiding Triggers
- Identify Triggers:
- Keep a diary to track what triggers your outbreaks. Common triggers include stress, illness, hormonal changes, sun exposure, and certain foods.
- Avoid Known Triggers:
- Once you identify your triggers, take steps to avoid them. For example, if sun exposure is a trigger, make sure to apply sunscreen regularly.
Antiviral Medications
- Prophylactic Antiviral Therapy:
- If you have frequent or severe outbreaks, your healthcare provider may prescribe daily antiviral medication such as acyclovir, valacyclovir, or famciclovir to reduce the frequency and severity of cold sores.
- Early Treatment:
- At the first sign of a cold sore (such as tingling or itching), start using antiviral creams or oral medications to reduce the severity and duration of the outbreak.
Boosting Immune System
- Stay Healthy:
- Maintain a healthy lifestyle to support your immune system. This includes regular exercise, a balanced diet, staying hydrated, and avoiding smoking and excessive alcohol consumption.
- Vaccinations:
- Stay up-to-date with vaccinations, especially for conditions that can weaken your immune system.
Preventing cold sores involves a multi-faceted approach that includes managing stress, protecting against sun exposure, maintaining good hygiene, recognizing and avoiding triggers, and possibly using antiviral medications. By adopting these preventive strategies, you can reduce the frequency and severity of cold sore outbreaks and maintain better overall health. If you experience frequent or severe outbreaks, consult a healthcare provider for personalized advice and treatment options.
Related Conditions
Cold sores, caused by the herpes simplex virus (HSV), can be associated with various related conditions due to the virus’s nature and the way it affects the body. Understanding these related conditions can provide a more comprehensive view of the potential implications of HSV infections. Here’s an overview of conditions related to cold sores:
- Herpes Simplex Virus Type 2 (HSV-2)
- Genital Herpes: While HSV-1 typically causes cold sores, HSV-2 primarily causes genital herpes. However, both types can infect the oral and genital areas. Genital herpes is characterized by painful sores and blisters in the genital region.
- Herpes Simplex Keratitis
- Eye Infection: HSV can infect the eye, causing herpes simplex keratitis. This condition affects the cornea and can lead to pain, redness, blurred vision, and in severe cases, vision loss. It often results from self-inoculation, where the virus is transferred from a cold sore to the eye.
- Herpetic Whitlow
- Finger Infection: Herpetic whitlow is an HSV infection of the fingers, often seen in healthcare workers or individuals who come into contact with the virus through open cuts or sores. It presents as painful, swollen sores on the fingers.
- Herpes Gladiatorum
- Skin Infection: Also known as “mat herpes,” this condition is common among athletes, particularly wrestlers. It results from skin-to-skin contact and manifests as blisters and sores on the body, including the face, neck, and arms.
- Eczema Herpeticum
- Severe Skin Infection: This serious condition occurs when HSV infects large areas of skin, often in individuals with pre-existing skin conditions like eczema. It can cause extensive, painful blisters and sores and requires prompt medical treatment.
- Herpes Encephalitis
- Brain Infection: Though rare, HSV can cause encephalitis, an inflammation of the brain. This condition can be life-threatening and presents with symptoms such as fever, headache, confusion, seizures, and neurological deficits.
- Neonatal Herpes
- Infant Infection: Newborns can acquire HSV from their mothers during childbirth, leading to neonatal herpes. This condition can cause severe systemic infection, affecting the skin, eyes, and internal organs, and can be life-threatening without prompt treatment.
- Bell’s Palsy
- Facial Nerve Paralysis: Although the exact cause is unknown, HSV-1 has been linked to Bell’s Palsy, a condition that causes sudden, temporary paralysis of one side of the face. Reactivation of the virus is thought to trigger inflammation of the facial nerve.
- Aphthous Ulcers (Canker Sores)
- Mouth Sores: While not caused by HSV, canker sores are often confused with cold sores. Unlike cold sores, canker sores occur inside the mouth and are not contagious. The exact cause of canker sores is unknown but may involve immune response, stress, or nutritional deficiencies.
- Chickenpox and Shingles
- Varicella-Zoster Virus (VZV): Related to HSV, VZV causes chickenpox in children and shingles (herpes zoster) in adults. Shingles occur due to reactivation of the VZV virus, similar to the reactivation seen with HSV.
Cold sores, caused by the herpes simplex virus, can be associated with a range of related conditions, from genital herpes and eye infections to more severe complications like herpes encephalitis and neonatal herpes. Understanding these related conditions helps in recognizing the broader impact of HSV infections and the importance of effective management and prevention strategies. If you experience symptoms of these related conditions, seeking medical advice for appropriate diagnosis and treatment is crucial.
Living With Cold Sores
Living with cold sores can be challenging due to their recurrent nature and the discomfort they cause. However, with effective management strategies, you can minimize the impact of cold sores on your daily life. Here are some tips and strategies to help you live with cold sores:
Managing Symptoms
- Early Treatment:
- At the first sign of a cold sore (such as tingling, itching, or burning), start treatment immediately with antiviral creams or oral medications prescribed by your healthcare provider. Early treatment can reduce the severity and duration of the outbreak.
- Pain Relief:
- Over-the-counter pain relievers like ibuprofen (Advil) or acetaminophen (Tylenol) can help alleviate pain and discomfort. Topical anesthetics such as lidocaine or benzocaine can also be applied directly to the sore.
- Cold Compresses:
- Applying a cold, damp cloth to the affected area can help reduce swelling and soothe pain.
- Avoid Irritants:
- Refrain from consuming acidic or spicy foods that can irritate cold sores. Stick to bland, soft foods if eating is painful.
Preventing Outbreaks
- Identify and Avoid Triggers:
- Keep a diary to track what triggers your outbreaks. Common triggers include stress, illness, sun exposure, hormonal changes, and certain foods. Once identified, take steps to avoid these triggers.
- Sun Protection:
- Use a broad-spectrum sunscreen with an SPF of 30 or higher on your face and lips when outdoors. Consider using a lip balm that contains sunscreen to protect your lips from UV rays.
- Stress Management:
- Practice stress-reducing techniques such as meditation, yoga, deep breathing exercises, and regular physical activity to help prevent outbreaks.
Maintaining Good Hygiene
- Hand Hygiene:
- Wash your hands frequently with soap and water, especially after touching your face or applying medication to a cold sore.
- Avoid Touching Sores:
- Try not to touch your cold sores unnecessarily to prevent spreading the virus to other parts of your body or to other people.
- Avoid Sharing Personal Items:
- Do not share items like lip balm, utensils, towels, or razors, as these can spread the herpes simplex virus.
Preventing Spread to Others
- Avoid Close Contact:
- Refrain from kissing or engaging in oral sex when you have an active cold sore to prevent spreading the virus to others.
- Use Separate Items:
- Use separate towels, utensils, and personal care items when you have a cold sore to reduce the risk of spreading the virus.
- Educate Partners:
- Inform your sexual partners about your condition so they can take precautions to avoid contracting the virus.
Long-Term Management
- Antiviral Medications:
- If you experience frequent or severe outbreaks, your healthcare provider may recommend daily antiviral medication to reduce the frequency and severity of cold sores.
- Regular Medical Check-Ups:
- Schedule regular visits with your healthcare provider to discuss your condition and any new treatment options that may be available.
Emotional Well-being
- Support Groups:
- Consider joining a support group for individuals with herpes simplex virus infections. Sharing experiences and coping strategies can be beneficial.
- Educate Yourself:
- Learn more about cold sores and their management to feel more in control of your condition. Knowledge can reduce anxiety and help you manage outbreaks more effectively.
- Stay Positive:
- Focus on the aspects of your life that are not affected by cold sores. Maintaining a positive outlook can help you cope with the condition more effectively.
Living with cold sores requires a combination of symptom management, preventive measures, good hygiene practices, and emotional support. By taking proactive steps to manage your condition and prevent outbreaks, you can reduce the impact of cold sores on your daily life. If you experience frequent or severe outbreaks, consult your healthcare provider for tailored treatment options and support.
Conclusion
In conclusion, cold sores, caused by the herpes simplex virus (HSV), can be a recurring challenge for those affected. These painful and often unsightly sores can impact daily life and emotional well-being. However, with effective management strategies, individuals can minimize the frequency and severity of outbreaks, as well as alleviate symptoms when they occur.
Understanding the triggers that lead to outbreaks, such as stress, illness, sun exposure, and hormonal changes, is crucial. By identifying and avoiding these triggers whenever possible, individuals can reduce the likelihood of cold sore recurrence. Good hygiene practices, including frequent handwashing and avoiding sharing personal items, also play a key role in preventing the spread of HSV.
Early treatment with antiviral medications, both oral and topical, can shorten the duration of outbreaks and alleviate discomfort. Pain relief measures such as cold compresses and over-the-counter medications can further help manage symptoms.
Maintaining overall health through adequate sleep, a balanced diet, regular exercise, and stress management techniques contributes to a strong immune system, which can in turn help prevent outbreaks. Sun protection, including the use of sunscreen and lip balms with SPF, is essential for reducing the impact of UV exposure, a common trigger for cold sores.
Living with cold sores involves not only physical management but also emotional support and education. Support groups and resources can provide valuable information and a sense of community for individuals navigating the challenges of HSV infections.
Ultimately, while cold sores may be a persistent part of life for some, proactive management and preventive measures can significantly improve quality of life and minimize the impact of outbreaks. Seeking guidance from healthcare providers for personalized treatment plans and staying informed about new developments in HSV management are essential steps toward effectively managing this condition.
