Kidney failure (renal failure), a condition characterized by the kidneys’ inability to adequately filter waste products and excess fluids from the blood, is a significant medical concern affecting millions of people worldwide. The kidneys play a crucial role in maintaining overall health by regulating fluid balance, electrolyte levels, and removing toxins from the body. When these vital organs fail, it can lead to severe health complications, necessitating immediate and ongoing medical intervention.
Kidney failure can manifest in two primary forms: acute kidney failure, which occurs suddenly and is often reversible, and chronic kidney failure, a gradual and typically irreversible condition that can lead to end-stage renal disease. Understanding the causes, symptoms, and treatment options for kidney failure is essential for effective management and prevention of this debilitating condition. This introduction delves into the multifaceted aspects of kidney failure, highlighting its impact on health and the importance of early detection and intervention.
Table of Contents
Types of Kidney Failure
Kidney failure, also known as renal failure, can be classified into two main types based on the duration and nature of the onset: acute kidney failure and chronic kidney failure. Each type has distinct causes, symptoms, and treatment approaches.
Acute Kidney Failure
Definition: Acute kidney failure, also known as acute renal failure (ARF) or acute kidney injury (AKI), is a sudden and often reversible decline in kidney function that occurs over a short period, typically within hours or days.
Causes:
- Dehydration: Severe loss of fluids, which can reduce blood flow to the kidneys.
- Sepsis: Severe infections leading to widespread inflammation and organ dysfunction.
- Acute Glomerulonephritis: Inflammation of the kidney’s filtering units, often due to immune responses.
- Obstruction of the Urinary Tract: Conditions like kidney stones, tumors, or an enlarged prostate that block urine flow.
- Medications and Toxins: Certain drugs, especially nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and contrast agents used in imaging studies, as well as toxins from infections or environmental exposure.
Symptoms:
- Decreased urine output
- Fluid retention causing swelling in the legs, ankles, and feet
- Shortness of breath
- Fatigue and confusion
- Nausea and vomiting
- Chest pain or pressure
Treatment:
- Addressing the underlying cause (e.g., treating infections, removing obstructions)
- Hydration and intravenous fluids to restore blood flow to the kidneys
- Medications to manage symptoms and prevent complications
- Dialysis, if necessary, to filter waste products from the blood until kidney function improves
Chronic Kidney Failure
Definition: Chronic kidney failure, also known as chronic kidney disease (CKD), is a gradual and progressive loss of kidney function over months or years. This condition is typically irreversible and can lead to end-stage renal disease (ESRD), requiring long-term dialysis or a kidney transplant.
Causes:
- Diabetes Mellitus: High blood sugar levels can damage kidney tissues over time.
- Hypertension: Chronic high blood pressure can cause blood vessel damage within the kidneys.
- Chronic Glomerulonephritis: Long-term inflammation of the kidney’s filtering units.
- Polycystic Kidney Disease: A genetic disorder characterized by the growth of numerous cysts in the kidneys.
- Prolonged Obstruction of the Urinary Tract: Long-term blockages that impair kidney function.
Symptoms:
- Increased or decreased urine output
- Swelling in the feet and ankles
- Persistent fatigue and weakness
- Loss of appetite and unintentional weight loss
- Persistent itching
- Sleep problems
- Muscle cramps
Treatment:
- Controlling underlying conditions like diabetes and hypertension through medications and lifestyle changes
- Dietary modifications to reduce the buildup of waste products in the blood
- Medications to manage symptoms and prevent further kidney damage
- Dialysis to perform the filtration functions of the kidneys
- Kidney transplant for suitable candidates to replace the failed kidneys with a healthy donor kidney
Understanding the differences between acute and chronic kidney failure is crucial for effective diagnosis and treatment. While acute kidney failure can often be reversed with prompt treatment, chronic kidney failure requires ongoing management to slow disease progression and address complications. Early detection and intervention are key to improving outcomes for individuals with either form of kidney failure.
Symptoms
Kidney failure, whether acute or chronic, manifests through a range of symptoms that can vary in severity based on the extent of kidney function loss. Recognizing these symptoms is crucial for timely diagnosis and treatment. Here are the common symptoms associated with both acute and chronic kidney failure:
Symptoms of Acute Kidney Failure
- Decreased Urine Output:
- A significant reduction in the amount of urine produced.
- Fluid Retention:
- Swelling in the legs, ankles, or feet due to the accumulation of fluids.
- Shortness of Breath:
- Difficulty breathing as fluid builds up in the lungs.
- Fatigue and Weakness:
- Feeling unusually tired or weak due to the buildup of waste products in the blood.
- Confusion or Difficulty Concentrating:
- Mental confusion or trouble focusing, which may be due to toxin accumulation.
- Nausea and Vomiting:
- Feeling nauseated or vomiting, often caused by the buildup of waste products.
- Chest Pain or Pressure:
- Discomfort in the chest, which can occur if fluid builds up around the heart lining.
- Seizures or Coma:
- In severe cases, acute kidney failure can lead to seizures or even coma.
Symptoms of Chronic Kidney Failure
- Increased or Decreased Urine Output:
- Changes in urination patterns, such as producing more or less urine than usual.
- Swelling in Feet and Ankles:
- Persistent swelling due to fluid retention.
- Persistent Fatigue and Weakness:
- Chronic tiredness and weakness due to the accumulation of waste products and anemia.
- Loss of Appetite:
- Reduced desire to eat, often accompanied by weight loss.
- Nausea and Vomiting:
- Ongoing nausea and vomiting due to toxin buildup.
- Sleep Problems:
- Difficulty sleeping, which may be due to muscle cramps or restless legs.
- Persistent Itching:
- Severe itching caused by waste products accumulating in the skin.
- Muscle Cramps:
- Cramping and twitching muscles, often due to electrolyte imbalances.
- High Blood Pressure (Hypertension):
- Elevated blood pressure that is difficult to control, contributing to further kidney damage.
- Shortness of Breath:
- Difficulty breathing, especially with exertion or lying down, due to fluid buildup.
- Chest Pain:
- Discomfort or pressure in the chest, which can be related to fluid overload or heart issues.
- Bone Pain and Fractures:
- Pain in bones or an increased risk of fractures due to mineral and bone disorders.
The symptoms of kidney failure, whether acute or chronic, can significantly impact a person’s quality of life. Early recognition of these symptoms and prompt medical intervention are essential for managing the condition effectively. Regular monitoring and appropriate treatment can help slow the progression of chronic kidney failure and improve outcomes for those with acute kidney failure.
Causes

Kidney failure can arise from a variety of underlying conditions and factors. The causes of kidney failure are generally categorized based on whether the condition is acute or chronic. Each type has distinct etiologies that contribute to the loss of kidney function.
Causes of Acute Kidney Failure
Acute kidney failure, also known as acute renal failure (ARF) or acute kidney injury (AKI), typically develops rapidly and can often be reversed if treated promptly. The main causes include:
- Prerenal Causes:
- Severe Dehydration: Significant loss of body fluids due to vomiting, diarrhea, or excessive sweating.
- Severe Blood Loss: Major bleeding from surgery or injury leading to reduced blood flow to the kidneys.
- Severe Infection (Sepsis): Body-wide infection causing a drastic drop in blood pressure and blood flow to the kidneys.
- Heart Failure: Reduced heart function leading to decreased blood flow to the kidneys.
- Intrarenal Causes:
- Acute Tubular Necrosis (ATN): Damage to the kidney’s tubule cells due to toxins or lack of oxygen.
- Glomerulonephritis: Inflammation of the kidney’s filtering units, often caused by infections or autoimmune diseases.
- Interstitial Nephritis: Inflammation of the kidney tissues, usually due to allergic reactions to medications or infections.
- Toxins: Exposure to nephrotoxic drugs (e.g., certain antibiotics, NSAIDs, and chemotherapy agents) or substances like heavy metals.
- Postrenal Causes:
- Urinary Tract Obstruction: Blockage of urine flow due to kidney stones, tumors, or an enlarged prostate.
- Bladder Dysfunction: Conditions that affect bladder emptying, such as neurogenic bladder.
Causes of Chronic Kidney Failure
Chronic kidney failure, also known as chronic kidney disease (CKD), progresses slowly over time and is often irreversible. The main causes include:
- Diabetes Mellitus:
- Diabetic Nephropathy: High blood sugar levels damage the kidneys’ filtering units, leading to chronic kidney damage.
- Hypertension:
- Hypertensive Nephrosclerosis: High blood pressure causes blood vessel damage within the kidneys, reducing their function over time.
- Glomerulonephritis:
- Chronic inflammation of the kidney’s filtering units due to autoimmune diseases, infections, or other causes.
- Polycystic Kidney Disease:
- A genetic disorder characterized by the growth of numerous cysts in the kidneys, leading to progressive loss of kidney function.
- Chronic Obstruction:
- Long-term blockage of the urinary tract, such as from kidney stones, tumors, or an enlarged prostate.
- Chronic Interstitial Nephritis:
- Long-term inflammation and scarring of the kidney’s interstitial tissue, often due to prolonged use of certain medications or infections.
- Vesicoureteral Reflux:
- A condition in which urine flows backward from the bladder into the kidneys, causing recurrent infections and scarring.
- Autoimmune Diseases:
- Conditions such as lupus or Goodpasture’s syndrome, where the body’s immune system attacks kidney tissues.
- Infections:
- Recurrent or chronic infections, such as chronic pyelonephritis, can lead to gradual kidney damage.
The causes of kidney failure are diverse and can be attributed to factors affecting the kidneys directly or indirectly through systemic conditions. Understanding these causes is crucial for early detection, prevention, and appropriate management of kidney failure. Regular health check-ups, effective management of underlying conditions like diabetes and hypertension, and avoiding nephrotoxic substances are key strategies to prevent or slow the progression of kidney failure.
Risk Factors
Kidney failure, whether acute or chronic, can be influenced by various risk factors that increase the likelihood of developing the condition. These risk factors can be broadly categorized into medical conditions, lifestyle choices, and genetic predispositions. Understanding these risk factors is crucial for prevention and early intervention.
Risk Factors for Acute Kidney Failure
- Advanced Age:
- Older adults are more susceptible to acute kidney injury due to the natural decline in kidney function with age.
- Preexisting Kidney Disease:
- Individuals with chronic kidney disease are at higher risk of experiencing acute kidney failure.
- Severe Infections or Sepsis:
- Severe infections can cause widespread inflammation and blood flow changes, leading to kidney injury.
- Major Surgery or Trauma:
- Surgery, especially procedures involving the heart or abdominal organs, and major injuries can reduce blood flow to the kidneys.
- Certain Medications:
- Use of nephrotoxic drugs such as NSAIDs, certain antibiotics, and contrast agents used in imaging studies can damage the kidneys.
- Dehydration:
- Severe dehydration from excessive fluid loss can lead to reduced blood flow to the kidneys.
- Heart Disease:
- Conditions such as heart failure and heart attack can reduce blood supply to the kidneys.
- Obstruction of the Urinary Tract:
- Kidney stones, tumors, or an enlarged prostate can block the flow of urine, causing acute kidney failure.
Risk Factors for Chronic Kidney Failure
- Diabetes Mellitus:
- High blood sugar levels over time can damage the kidneys, leading to diabetic nephropathy.
- Hypertension (High Blood Pressure):
- Chronic high blood pressure can cause damage to the blood vessels in the kidneys, reducing their function.
- Cardiovascular Disease:
- Conditions affecting the heart and blood vessels can impair kidney function.
- Family History of Kidney Disease:
- Genetic predispositions, such as polycystic kidney disease, can increase the risk of chronic kidney failure.
- Obesity:
- Excess body weight is associated with an increased risk of developing conditions like diabetes and hypertension, which are risk factors for kidney disease.
- Smoking:
- Smoking can damage blood vessels and decrease blood flow to the kidneys, contributing to kidney damage.
- Age:
- The risk of chronic kidney disease increases with age due to the natural decline in kidney function.
- Autoimmune Diseases:
- Conditions like lupus and rheumatoid arthritis can lead to chronic inflammation and kidney damage.
- Prolonged Use of Certain Medications:
- Long-term use of drugs that are toxic to the kidneys, such as some painkillers and anti-inflammatory medications, can lead to chronic kidney damage.
- Chronic Urinary Tract Infections:
- Repeated infections can cause scarring and damage to the kidneys over time.
- Ethnicity:
- Certain ethnic groups, such as African Americans, Hispanics, and Native Americans, have a higher risk of developing chronic kidney disease.
Recognizing and addressing risk factors for kidney failure is crucial for prevention and early intervention. Regular health check-ups, effective management of conditions like diabetes and hypertension, maintaining a healthy lifestyle, and avoiding nephrotoxic substances are key strategies to reduce the risk of kidney failure. Early detection and management of risk factors can significantly improve outcomes for individuals at risk of both acute and chronic kidney failure.
Diagnosis
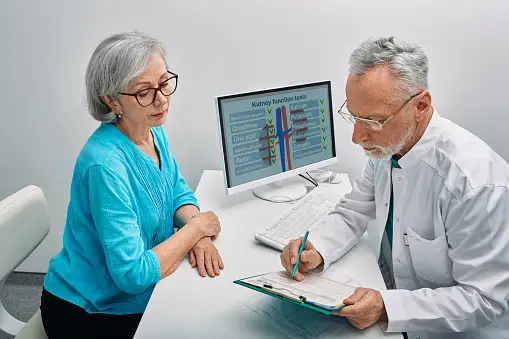
Diagnosing kidney failure involves a combination of clinical evaluation, laboratory tests, and imaging studies. Early and accurate diagnosis is crucial for managing the condition effectively and preventing further kidney damage. Here are the key diagnostic approaches:
Clinical Evaluation
- Medical History:
- Detailed history of symptoms, duration, and severity.
- Past medical conditions such as diabetes, hypertension, infections, and family history of kidney disease.
- Medication history, including use of nephrotoxic drugs.
- Physical Examination:
- Checking for signs of fluid retention (e.g., swelling in the legs, ankles, or feet).
- Assessing blood pressure, heart rate, and respiratory status.
- Evaluating for signs of underlying conditions (e.g., skin rashes in autoimmune diseases, signs of infection).
Laboratory Tests
- Blood Tests:
- Serum Creatinine: Elevated levels indicate reduced kidney function.
- Blood Urea Nitrogen (BUN): Increased levels suggest impaired kidney function.
- Glomerular Filtration Rate (GFR): Estimated from serum creatinine levels to assess kidney function.
- Electrolytes: Abnormal levels of potassium, sodium, and other electrolytes indicate kidney dysfunction.
- Complete Blood Count (CBC): Anemia or infection can be detected through changes in blood cell counts.
- Urine Tests:
- Urinalysis: Examines urine for abnormalities such as protein, blood, glucose, and infection.
- Urine Protein-to-Creatinine Ratio: Measures the amount of protein in the urine to detect kidney damage.
- 24-hour Urine Collection: Quantifies urine output and protein excretion over 24 hours.
Imaging Studies
- Ultrasound:
- A non-invasive imaging technique that assesses the size, shape, and structure of the kidneys.
- Detects obstructions (e.g., kidney stones), cysts, tumors, and other abnormalities.
- CT Scan (Computed Tomography):
- Provides detailed images of the kidneys and urinary tract.
- Useful for identifying obstructions, masses, and structural abnormalities.
- MRI (Magnetic Resonance Imaging):
- Offers detailed images without radiation exposure.
- Helpful in evaluating complex kidney conditions.
- Renal Scintigraphy:
- A nuclear medicine test that evaluates kidney function and blood flow.
Specialized Tests
- Kidney Biopsy:
- Involves taking a small sample of kidney tissue for microscopic examination.
- Helps diagnose specific kidney diseases (e.g., glomerulonephritis, interstitial nephritis) and determine the extent of damage.
- Renal Angiography:
- An imaging test that visualizes the blood vessels of the kidneys using a contrast dye.
- Used to assess blood flow and identify vascular abnormalities.
The diagnosis of kidney failure requires a comprehensive approach that includes clinical evaluation, laboratory tests, and imaging studies. Early detection and accurate diagnosis are essential for effective management and treatment. Regular monitoring and follow-up are crucial for individuals at risk of kidney failure or those with existing kidney conditions to prevent further progression and complications.
Treatment
The treatment of kidney failure depends on whether it is acute or chronic, as well as the underlying cause and severity of the condition. Here are the main treatment approaches for both acute kidney failure and chronic kidney failure:
Treatment of Acute Kidney Failure
1. Addressing Underlying Causes:
- Dehydration: Intravenous (IV) fluids to restore hydration and blood flow to the kidneys.
- Infections: Antibiotics to treat underlying infections.
- Obstruction Removal: Procedures to remove or bypass urinary obstructions (e.g., kidney stones, tumors).
- Medication Adjustments: Stopping or adjusting doses of nephrotoxic drugs.
2. Supporting Kidney Function:
- Dialysis: Temporary dialysis may be necessary to remove waste products and excess fluids from the blood until kidney function improves.
- Electrolyte Management: Correcting imbalances in electrolytes, such as potassium and sodium, through medications or dietary changes.
3. Managing Symptoms:
- Medications: Drugs to manage symptoms like nausea, high blood pressure, and fluid overload.
- Nutritional Support: Dietary modifications to limit protein, potassium, and sodium intake to reduce the burden on the kidneys.
Treatment of Chronic Kidney Failure
1. Managing Underlying Conditions:
- Diabetes Control: Tight blood sugar control through medications, insulin, and lifestyle changes to prevent further kidney damage.
- Hypertension Management: Medications such as ACE inhibitors or angiotensin II receptor blockers (ARBs) to control blood pressure and protect kidney function.
2. Slowing Disease Progression:
- Dietary Changes: Low-protein diet to reduce waste buildup, and limiting salt and potassium intake.
- Medications: Drugs to manage complications such as anemia (erythropoiesis-stimulating agents), bone disease (phosphate binders, vitamin D supplements), and fluid overload (diuretics).
3. Treating Complications:
- Anemia: Iron supplements and erythropoiesis-stimulating agents to boost red blood cell production.
- Bone and Mineral Disorders: Phosphate binders and vitamin D analogs to manage calcium and phosphate levels.
- Acidosis: Sodium bicarbonate to correct acid-base imbalances.
4. Renal Replacement Therapy:
- Dialysis:
- Hemodialysis: Blood is filtered through a machine to remove waste products and excess fluids.
- Peritoneal Dialysis: The peritoneal cavity is used as a natural filter by infusing a dialysis solution that absorbs waste products and excess fluids.
- Kidney Transplant: Surgical procedure to replace the failed kidney with a healthy donor kidney. It is the most effective treatment for end-stage renal disease (ESRD) but requires a suitable donor and lifelong immunosuppressive medications to prevent rejection.
5. Lifestyle Modifications:
- Smoking Cessation: Quitting smoking to improve overall health and kidney function.
- Exercise: Regular physical activity to maintain a healthy weight and control blood pressure.
- Healthy Diet: Following a kidney-friendly diet to manage symptoms and prevent complications.
Treatment for kidney failure involves a multifaceted approach tailored to the type and severity of the condition. For acute kidney failure, the focus is on addressing the underlying cause and supporting kidney function until recovery. For chronic kidney failure, managing underlying conditions, slowing disease progression, treating complications, and considering renal replacement therapy are key components. Early diagnosis, regular monitoring, and adherence to treatment plans are crucial for improving outcomes and quality of life for individuals with kidney failure.
How to Prevent Kidney Failure
Preventing kidney failure involves taking steps to maintain kidney health and managing underlying conditions that can lead to kidney damage. Here are comprehensive strategies to prevent both acute and chronic kidney failure:
1. Maintain a Healthy Lifestyle
a. Diet:
- Eat a Balanced Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins.
- Limit Sodium Intake: Reduce salt intake to manage blood pressure and prevent fluid retention.
- Control Protein Intake: Avoid excessive protein consumption, especially for individuals with early kidney disease.
- Stay Hydrated: Drink adequate water to help kidneys function properly, but avoid excessive fluid intake that can stress the kidneys.
b. Exercise:
- Regular Physical Activity: Engage in at least 30 minutes of moderate exercise most days of the week to maintain a healthy weight and manage blood pressure.
c. Avoid Smoking and Limit Alcohol:
- Quit Smoking: Smoking damages blood vessels and reduces blood flow to the kidneys.
- Limit Alcohol: Excessive alcohol can cause dehydration and high blood pressure, both of which can harm the kidneys.
2. Manage Medical Conditions
a. Diabetes:
- Blood Sugar Control: Keep blood sugar levels within target range through diet, exercise, and medications if necessary.
- Regular Monitoring: Frequent check-ups with a healthcare provider to monitor kidney function and manage diabetes effectively.
b. Hypertension:
- Blood Pressure Management: Maintain blood pressure within normal limits through diet, exercise, and antihypertensive medications if needed.
- Regular Monitoring: Regular blood pressure checks and adherence to prescribed medications.
c. Heart Disease:
- Heart Health: Manage cholesterol levels, maintain a healthy weight, and follow a heart-healthy diet.
3. Avoid Nephrotoxic Substances
a. Medications:
- Use Medications Wisely: Avoid overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) and other medications that can harm the kidneys.
- Consult Healthcare Providers: Always consult with healthcare providers before starting new medications, especially if you have existing kidney concerns.
b. Toxins:
- Avoid Exposure: Minimize exposure to environmental toxins and chemicals that can damage the kidneys.
4. Regular Health Check-ups
a. Routine Screening:
- Check Kidney Function: Regular blood tests (e.g., serum creatinine, GFR) and urine tests (e.g., urine protein) to monitor kidney health.
- Early Detection: Early identification and management of kidney problems can prevent progression to kidney failure.
5. Manage Infections and Obstructions
a. Prevent Infections:
- Hygiene: Maintain good personal hygiene to prevent urinary tract infections (UTIs).
- Seek Treatment Promptly: Treat infections promptly to prevent them from spreading to the kidneys.
b. Address Obstructions:
- Manage Urinary Issues: Promptly address any urinary tract obstructions or issues, such as kidney stones or an enlarged prostate.
6. Genetic and Family History Awareness
a. Know Your Risk:
- Family History: Be aware of any family history of kidney disease or conditions that can lead to kidney failure.
- Genetic Counseling: Consider genetic counseling if you have a family history of hereditary kidney diseases, like polycystic kidney disease.
Preventing kidney failure involves a proactive approach to overall health and well-being. By adopting a healthy lifestyle, managing medical conditions, avoiding nephrotoxic substances, and undergoing regular health check-ups, individuals can significantly reduce their risk of developing kidney failure. Early intervention and consistent management are key to maintaining kidney health and preventing the progression of kidney disease.
Related Conditions
Kidney failure is often associated with a range of related conditions that can either contribute to its development or arise as complications due to impaired kidney function. Understanding these related conditions is crucial for comprehensive management and prevention strategies.
Conditions Contributing to Kidney Failure
- Diabetes Mellitus:
- Description: A chronic condition characterized by high blood sugar levels.
- Impact: Long-term uncontrolled diabetes can damage the blood vessels in the kidneys, leading to diabetic nephropathy, a common cause of chronic kidney failure.
- Hypertension (High Blood Pressure):
- Description: Persistent elevation of blood pressure in the arteries.
- Impact: High blood pressure can cause damage to the blood vessels in the kidneys, reducing their ability to function properly.
- Cardiovascular Disease:
- Description: Conditions affecting the heart and blood vessels, such as coronary artery disease and heart failure.
- Impact: Reduced blood flow to the kidneys due to heart problems can lead to kidney damage and failure.
- Chronic Glomerulonephritis:
- Description: Inflammation of the kidney’s filtering units (glomeruli).
- Impact: Can lead to scarring and eventual kidney failure.
- Polycystic Kidney Disease:
- Description: A genetic disorder characterized by the growth of numerous cysts in the kidneys.
- Impact: Over time, these cysts can enlarge and damage kidney tissue, leading to chronic kidney failure.
- Urinary Tract Obstructions:
- Description: Blockages in the urinary tract, such as kidney stones, tumors, or an enlarged prostate.
- Impact: Obstructions can lead to kidney damage by increasing pressure in the urinary tract and reducing urine flow.
Conditions Resulting from Kidney Failure
- Anemia:
- Description: A condition characterized by a deficiency of red blood cells.
- Impact: Kidneys produce erythropoietin, a hormone that stimulates red blood cell production. Kidney failure reduces erythropoietin levels, leading to anemia.
- Bone and Mineral Disorders:
- Description: Imbalances in calcium, phosphate, and vitamin D metabolism.
- Impact: Impaired kidney function disrupts the balance of these minerals, leading to bone diseases such as osteodystrophy.
- Electrolyte Imbalances:
- Description: Abnormal levels of electrolytes like potassium, sodium, and phosphorus.
- Impact: Can cause a range of symptoms, including muscle cramps, fatigue, heart arrhythmias, and in severe cases, cardiac arrest.
- Fluid Overload:
- Description: Excess fluid accumulation in the body.
- Impact: Can cause swelling (edema), high blood pressure, and pulmonary edema (fluid in the lungs), leading to difficulty breathing.
- Cardiovascular Disease:
- Description: Increased risk of heart disease and stroke.
- Impact: Kidney failure can contribute to cardiovascular problems due to hypertension, fluid overload, and metabolic imbalances.
- Hyperkalemia:
- Description: High levels of potassium in the blood.
- Impact: Can lead to dangerous heart rhythms and cardiac arrest.
- Metabolic Acidosis:
- Description: Accumulation of acid in the body due to the kidneys’ inability to excrete hydrogen ions.
- Impact: Can cause rapid breathing, fatigue, confusion, and in severe cases, shock or death.
- Uremia:
- Description: Accumulation of waste products in the blood.
- Impact: Can lead to symptoms such as nausea, vomiting, fatigue, confusion, and pruritus (itching). Severe uremia requires dialysis.
Kidney failure is closely linked to a variety of conditions that can either precipitate its onset or emerge as complications of diminished kidney function. Effective management of these related conditions is critical to preventing kidney failure and mitigating its impact on overall health. Regular monitoring, early intervention, and comprehensive treatment plans are essential for addressing both the causes and consequences of kidney failure.
Living With Kidney Failure
Living with kidney failure requires significant lifestyle adjustments and proactive management to maintain health and quality of life. Here are key considerations and strategies for individuals living with kidney failure:
Medical Management
- Regular Monitoring:
- Frequent Check-ups: Regular visits to a nephrologist to monitor kidney function and manage complications.
- Blood Tests: Routine blood tests to check for electrolyte imbalances, anemia, and other kidney-related issues.
- Medications:
- Prescribed Medications: Adherence to medications prescribed for blood pressure control, anemia, bone health, and other conditions.
- Avoid Nephrotoxic Drugs: Consult healthcare providers before taking new medications or over-the-counter drugs to avoid those harmful to kidneys.
- Dialysis:
- Hemodialysis: Regular sessions to filter waste products and excess fluids from the blood.
- Peritoneal Dialysis: Daily or multiple daily exchanges using the peritoneal cavity to remove waste products and fluids.
- Kidney Transplant:
- Transplant Evaluation: Assessment for eligibility for a kidney transplant.
- Post-Transplant Care: Lifelong immunosuppressive medications and regular monitoring to prevent rejection.
Dietary Modifications
- Fluid Intake:
- Fluid Restrictions: Limiting fluid intake to prevent fluid overload and swelling.
- Dietary Restrictions:
- Low Sodium: Reducing salt intake to manage blood pressure and fluid retention.
- Low Potassium: Avoiding high-potassium foods (e.g., bananas, oranges, potatoes) to prevent hyperkalemia.
- Low Phosphorus: Limiting phosphorus-rich foods (e.g., dairy products, nuts, beans) to protect bone health.
- Protein Management: Consuming moderate amounts of high-quality protein to minimize waste buildup while maintaining nutritional needs.
- Nutritional Support:
- Dietitian Consultation: Working with a renal dietitian to develop a personalized eating plan that meets nutritional needs while adhering to dietary restrictions.
Lifestyle Adjustments
- Exercise:
- Regular Physical Activity: Engaging in appropriate exercise to maintain overall health and manage weight.
- Customized Fitness Plans: Tailoring exercise routines to individual capabilities and restrictions.
- Smoking and Alcohol:
- Quit Smoking: Avoiding tobacco to improve cardiovascular health and reduce further kidney damage.
- Limit Alcohol: Reducing or eliminating alcohol consumption to prevent additional strain on the kidneys.
- Mental Health:
- Counseling and Support Groups: Seeking psychological support to cope with the emotional challenges of living with kidney failure.
- Stress Management: Practicing relaxation techniques, such as meditation and yoga, to manage stress and anxiety.
Managing Complications
- Anemia:
- Iron Supplements: Taking iron supplements and erythropoiesis-stimulating agents as prescribed to manage anemia.
- Regular Monitoring: Monitoring hemoglobin levels to ensure effective treatment.
- Bone and Mineral Disorders:
- Phosphate Binders: Taking medications to control phosphorus levels.
- Vitamin D Supplements: Supplementing with active vitamin D to maintain bone health.
- Cardiovascular Health:
- Blood Pressure Control: Maintaining target blood pressure levels through medications and lifestyle changes.
- Regular Heart Check-ups: Monitoring cardiovascular health to prevent complications.
Emergency Preparedness
- Medical Information:
- Medical ID: Wearing a medical identification bracelet indicating kidney failure and dialysis status.
- Emergency Contacts: Keeping a list of emergency contacts and medical information readily accessible.
- Emergency Plans:
- Dialysis Backup Plans: Knowing alternative dialysis centers and having a plan for dialysis during emergencies (e.g., natural disasters).
Living with kidney failure involves a multifaceted approach to health management, including medical treatments, dietary adjustments, lifestyle changes, and mental health support. By adhering to medical advice, maintaining a healthy lifestyle, and proactively managing complications, individuals with kidney failure can improve their quality of life and outcomes. Regular communication with healthcare providers and support networks is essential for navigating the challenges of kidney failure.
