Hepatitis A, a highly contagious liver infection caused by the hepatitis A virus (HAV), is a significant global health concern. This virus primarily spreads through ingestion of contaminated food or water, or through close contact with an infected person. Hepatitis A affects millions of people worldwide annually, with outbreaks occurring in regions with poor sanitation or during foodborne transmission events.
Despite being preventable with vaccination and good hygiene practices, hepatitis A remains a public health challenge due to its potential to cause acute liver inflammation, leading to jaundice, fatigue, and in severe cases, liver failure. Understanding the transmission, symptoms, prevention, and treatment of hepatitis A is crucial in mitigating its impact on individuals and communities globally.
Table of Contents
Symptoms of Hepatitis A
Hepatitis A is an infectious liver disease caused by the hepatitis A virus (HAV). The symptoms of hepatitis A can vary in severity and typically develop within 2 to 6 weeks after exposure to the virus. Here are the common symptoms associated with hepatitis A:
- Jaundice: Yellowing of the skin and whites of the eyes is a hallmark symptom of hepatitis A, caused by elevated bilirubin levels in the bloodstream.
- Fatigue: Persistent tiredness and lack of energy are common early symptoms of hepatitis A, often preceding other symptoms.
- Abdominal Pain: Discomfort or pain in the upper right side of the abdomen may occur as the liver becomes inflamed.
- Loss of Appetite: A reduced desire to eat or early feelings of fullness can accompany hepatitis A infection.
- Nausea and Vomiting: Digestive symptoms such as nausea and vomiting may occur, particularly in the early stages of the illness.
- Fever: Low-grade fever is common and may fluctuate throughout the course of the infection.
- Dark Urine: Urine may appear dark yellow or brown due to increased levels of bilirubin.
- Pale Stools: Stools may become pale or clay-colored as a result of reduced bile production.
- Joint Pain: Some individuals may experience joint pain, which can be a less common symptom of hepatitis A.
- Itching: Itching of the skin (pruritus) may occur, especially in cases of prolonged jaundice.
The severity of symptoms can vary widely, with some individuals experiencing mild illness and others developing more severe complications such as liver failure. It’s important to seek medical attention if symptoms of hepatitis A are present, especially if there is known exposure to the virus or if symptoms worsen over time. Prompt diagnosis and appropriate medical care can help manage symptoms and prevent complications associated with hepatitis A infection.
Causes of Hepatitis A
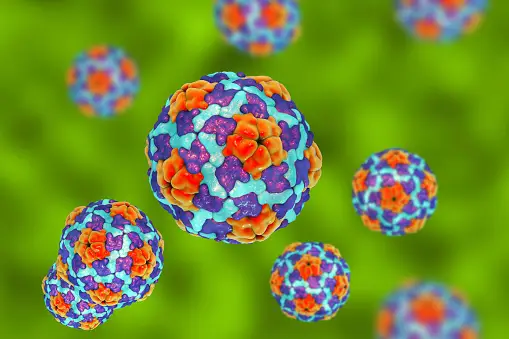
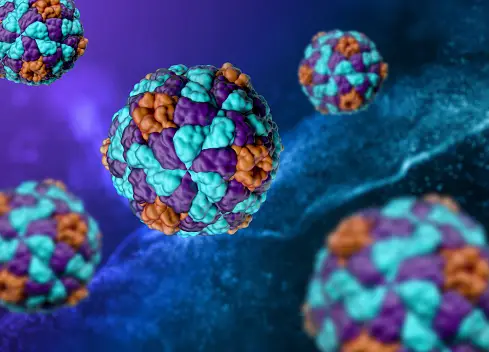
Hepatitis A is caused by infection with the hepatitis A virus (HAV), which belongs to the Picornaviridae family. The virus primarily affects the liver and is transmitted through ingestion of contaminated food or water or through close contact with an infected person. Here are the key causes and modes of transmission of hepatitis A:
- Contaminated Food and Water: Hepatitis A virus can survive in contaminated water and food, especially in areas with poor sanitation or inadequate hygiene practices. Consuming raw or undercooked shellfish from contaminated waters is a common source of infection.
- Close Personal Contact: The virus can spread through close contact with an infected person, particularly in settings where personal hygiene is compromised or in crowded living conditions. This includes sharing food, utensils, or engaging in sexual activities with an infected individual.
- Poor Sanitation: Areas with inadequate sanitation facilities and poor hygiene practices increase the risk of hepatitis A transmission. Lack of clean drinking water and improper disposal of sewage can contribute to outbreaks of the virus.
- Travel to Endemic Areas: Travelers to regions with high rates of hepatitis A, especially countries with poor sanitation standards, are at increased risk of infection. This includes travelers to parts of Africa, Asia, Central and South America, and Eastern Europe.
- Outbreaks: Hepatitis A outbreaks can occur in communities, institutions (such as schools or childcare centers), or in settings where there is close contact and shared facilities, amplifying the spread of the virus.
Understanding these modes of transmission is crucial in implementing preventive measures such as vaccination, practicing good personal hygiene, and ensuring food and water safety to reduce the risk of hepatitis A infection.
Risk Factors for Hepatitis A
Several factors increase the likelihood of contracting hepatitis A virus (HAV) infection. Understanding these risk factors can help individuals and communities take preventive measures to reduce the spread of the virus. Here are the main risk factors associated with hepatitis A:
- Travel to Endemic Areas: Travelers visiting regions with high rates of hepatitis A, especially countries with inadequate sanitation and hygiene practices, are at increased risk. This includes parts of Africa, Asia, Central and South America, and Eastern Europe.
- Close Contact with Infected Individuals: Hepatitis A spreads through direct contact with an infected person, particularly in settings where personal hygiene is compromised. Sharing food, drinks, or engaging in sexual activities with an infected individual increases the risk of transmission.
- Poor Sanitation and Hygiene: Living in or visiting areas with inadequate sanitation infrastructure increases the likelihood of exposure to contaminated food, water, or environmental surfaces harboring the virus.
- Occupational Exposure: Certain occupations, such as healthcare workers, daycare workers, and food handlers, may have an increased risk of exposure to hepatitis A due to close contact with infected individuals or contaminated materials.
- Injection Drug Use: People who inject drugs are at higher risk of hepatitis A infection due to sharing needles, syringes, or other drug paraphernalia contaminated with the virus.
- Men who have Sex with Men (MSM): MSM are at increased risk of hepatitis A infection due to higher rates of sexual transmission, particularly in communities or environments where hepatitis A is prevalent.
- Household or Sexual Contacts of Infected Individuals: Close household or sexual contacts of individuals diagnosed with hepatitis A are at elevated risk of infection due to direct exposure to the virus.
- Chronic Liver Disease: Individuals with pre-existing chronic liver disease, such as hepatitis B or hepatitis C, are at higher risk of complications from hepatitis A infection.
Diagnosis of Hepatitis A

Diagnosing hepatitis A involves a combination of medical history assessment, physical examination, and laboratory tests to confirm the presence of hepatitis A virus (HAV) infection. Here are the main steps involved in diagnosing hepatitis A:
- Medical History and Physical Examination:
- Symptoms Assessment: The doctor will inquire about symptoms such as jaundice (yellowing of the skin and eyes), fatigue, abdominal pain, nausea, dark urine, and pale stools.
- Risk Factors: Discussion about recent travel history to endemic areas, exposure to contaminated food or water, close contact with infected individuals, or high-risk behaviors like injection drug use or unprotected sexual activity.
- Laboratory Tests:
- HAV IgM Antibody Test: This blood test detects immunoglobulin M (IgM) antibodies produced by the immune system in response to HAV infection. IgM antibodies are typically detectable early in the infection and indicate acute hepatitis A.
- Liver Function Tests (LFTs): Blood tests to assess liver enzyme levels (such as ALT and AST) and bilirubin levels. Elevated liver enzymes and bilirubin are indicative of liver inflammation and dysfunction.
- Total and Direct Bilirubin: Levels of bilirubin in the blood are measured to assess the severity of jaundice.
- Imaging Studies:
- Imaging tests such as ultrasound or CT scan may be performed to evaluate the liver’s size, shape, and detect any abnormalities that could indicate complications of hepatitis A, such as liver enlargement or gallbladder issues.
- Liver Biopsy (Rarely Needed):
- In some cases, a liver biopsy may be performed to assess the extent of liver damage and rule out other liver conditions. A small sample of liver tissue is removed for microscopic examination.
Differential Diagnosis
The diagnosis of hepatitis A involves distinguishing it from other causes of acute hepatitis, such as hepatitis B, hepatitis C, autoimmune hepatitis, drug-induced liver injury, and other viral infections.
Diagnosing hepatitis A relies on a thorough clinical evaluation, specific blood tests to detect HAV antibodies, and assessment of liver function. Early diagnosis is crucial for initiating appropriate medical management, monitoring liver health, and preventing complications associated with acute hepatitis A infection. If symptoms suggestive of hepatitis A are present, seeking medical attention promptly is essential for accurate diagnosis and timely treatment.
Treatment of Hepatitis A

Treatment for hepatitis A focuses on managing symptoms, supporting liver function, and allowing the body to fight off the infection naturally. Here are the main aspects of treatment for hepatitis A:
- Supportive Care:
- Rest: Adequate rest is essential to help the body recover and conserve energy.
- Hydration: Drinking plenty of fluids helps prevent dehydration, especially if there is vomiting or diarrhea.
- Nutrition:
- Healthy Diet: Eating a balanced diet with adequate calories and nutrients supports overall health and liver function. Avoiding alcohol is crucial as it can worsen liver inflammation.
- Symptom Management:
- Medications: Over-the-counter medications such as acetaminophen (paracetamol) should be avoided unless prescribed by a doctor, as they can affect liver function.
- Itching: If itching occurs due to jaundice, antihistamines or medications prescribed by a doctor may provide relief.
- Monitoring and Follow-Up:
- Liver Function Tests: Regular monitoring of liver enzymes and bilirubin levels helps track the progression of hepatitis A and assess liver health.
- Medical Evaluation: Follow-up appointments with a healthcare provider are important to monitor recovery and ensure there are no complications.
- Prevention of Spread:
- Hygiene: Practicing good hygiene, including frequent handwashing, especially after using the bathroom and before preparing or eating food, helps prevent the spread of hepatitis A to others.
- Isolation: Infected individuals should avoid close personal contact with others until they are no longer contagious, which typically occurs about 1-2 weeks after the onset of symptoms.
- Vaccination:
- Post-exposure Prophylaxis: People who have been exposed to hepatitis A and have not been vaccinated previously may benefit from a hepatitis A vaccine or immune globulin within 2 weeks of exposure to prevent infection or lessen its severity.
Recovery and Prognosis
Most people with hepatitis A recover completely with supportive care and do not develop long-term liver damage. The acute phase of hepatitis A typically lasts a few weeks to months, after which symptoms improve as the body clears the virus. However, in rare cases, hepatitis A can lead to fulminant hepatitis (severe liver failure), especially in older adults or individuals with pre-existing liver disease.
Treatment for hepatitis A is primarily supportive, focusing on managing symptoms, maintaining hydration and nutrition, and preventing complications. Early diagnosis, adequate rest, and following medical advice are crucial for a smooth recovery from hepatitis A. Vaccination remains the most effective preventive measure against hepatitis A, emphasizing the importance of vaccination programs in reducing the incidence and impact of the disease globally.
Prevention of Hepatitis A

Preventing hepatitis A primarily involves vaccination, practicing good hygiene, and being cautious about food and water sources. Here are the key preventive measures:
- Vaccination:
- Hepatitis A Vaccine: Vaccination against hepatitis A is highly effective in preventing infection. The vaccine is recommended for:
- Travelers: Especially to regions with high rates of hepatitis A.
- Children: Routine vaccination is recommended in many countries, typically starting at age 1 or 2.
- High-Risk Groups: Including individuals with chronic liver disease, men who have sex with men (MSM), and people who use injection drugs.
- Post-exposure Prophylaxis: For those who have been exposed to hepatitis A and have not been vaccinated previously, vaccination or immune globulin can prevent infection or reduce its severity if administered within 2 weeks of exposure.
- Hepatitis A Vaccine: Vaccination against hepatitis A is highly effective in preventing infection. The vaccine is recommended for:
- Good Hygiene Practices:
- Handwashing: Wash hands thoroughly with soap and water, especially after using the bathroom, changing diapers, and before preparing or eating food.
- Safe Food and Water: Avoid consuming raw or undercooked shellfish, and ensure that drinking water is safe and from a reliable source. When traveling to areas with questionable water quality, drink bottled water and avoid ice cubes made from tap water.
- Personal and Environmental Hygiene:
- Sanitation: Maintain cleanliness in living spaces, particularly in bathrooms and kitchens, to prevent the spread of hepatitis A virus.
- Avoid Sharing Personal Items: Do not share personal items such as towels, toothbrushes, or razors, which can potentially spread the virus.
- Education and Awareness:
- Community Education: Increase awareness about hepatitis A transmission, symptoms, and prevention measures through public health campaigns, healthcare providers, and community organizations.
- High-Risk Groups: Target interventions and vaccination efforts towards populations at higher risk of hepatitis A infection, such as travelers, MSM, and individuals living in crowded or unsanitary conditions.
- Outbreak Response:
- Prompt Public Health Response: During outbreaks or clusters of hepatitis A cases, public health authorities should implement measures such as vaccination campaigns, sanitation improvements, and education to control the spread of the virus.
Preventing hepatitis A involves a combination of vaccination, good personal hygiene practices, and safe food and water habits. Vaccination is the cornerstone of prevention, providing long-term protection against hepatitis A infection. Practicing these preventive measures not only reduces individual risk but also contributes to public health efforts in controlling and eliminating hepatitis A worldwide.
Complications of Hepatitis A
Hepatitis A is typically a self-limited disease that resolves on its own without causing long-term liver damage in most cases. However, in some instances, especially in older adults or individuals with pre-existing liver disease, hepatitis A can lead to complications. Here are the potential complications associated with hepatitis A:
- Fulminant Hepatitis:
- Description: Fulminant hepatitis is a rare but severe complication where there is rapid and massive liver failure.
- Risk Factors: Older adults and individuals with chronic liver disease are at higher risk.
- Symptoms: Severe jaundice, confusion, bleeding tendencies, and coma may develop rapidly.
- Management: Requires intensive medical care, and liver transplantation may be necessary in severe cases.
- Cholestatic Hepatitis:
- Description: Cholestatic hepatitis occurs when there is impairment of bile flow from the liver, leading to bile accumulation and liver cell injury.
- Symptoms: Prolonged jaundice, severe itching (pruritus), and light-colored stools.
- Management: Supportive care to manage symptoms and monitor liver function until bile flow is restored.
- Relapsing Hepatitis:
- Description: Some individuals may experience a relapse of hepatitis A symptoms after an initial improvement.
- Symptoms: Recurrence of jaundice, fatigue, and other symptoms of hepatitis A.
- Management: Requires supportive care similar to the initial phase of infection.
- Extrahepatic Manifestations:
- Description: Hepatitis A can occasionally lead to extrahepatic complications affecting organs outside the liver.
- Examples: These may include kidney inflammation (glomerulonephritis), pancreatitis (inflammation of the pancreas), and autoimmune disorders triggered by the infection.
- Long-Term Sequelae:
- Description: While rare, hepatitis A infection has been associated with prolonged fatigue and autoimmune hepatitis, where the immune system mistakenly attacks the liver after the initial infection has cleared.
- Management: Requires ongoing medical management to address symptoms and monitor liver health.
Prevention of Complications
Preventing complications of hepatitis A primarily involves early diagnosis, supportive care during the acute phase of infection, and appropriate medical management for individuals at risk of severe disease. Vaccination against hepatitis A is highly effective in preventing infection and reducing the risk of complications, especially in high-risk populations. Prompt medical attention and adherence to preventive measures are crucial in minimizing the impact of hepatitis A and ensuring optimal recovery.
Living With Hepatitis A
Living with hepatitis A generally involves managing symptoms and allowing the body to recover from the infection, as it is typically a self-limited disease that resolves on its own without causing chronic liver damage in most cases. Here are some key aspects of living with hepatitis A:
During the Acute Phase:
- Symptom Management:
- Rest: Adequate rest is crucial to support the body’s recovery process.
- Hydration: Drink plenty of fluids to stay hydrated, especially if experiencing vomiting or diarrhea.
- Nutrition: Eat a balanced diet to support liver function and overall health. Avoid alcohol and fatty foods that may stress the liver.
- Medication Use:
- Avoid Certain Medications: Over-the-counter medications such as acetaminophen (paracetamol) should be avoided unless recommended by a healthcare provider, as they can affect liver function.
- Monitoring:
- Liver Function Tests: Your doctor may monitor liver enzymes and bilirubin levels through blood tests to track recovery and ensure there are no complications.
Recovery Phase:
- Follow-Up Care:
- Medical Appointments: Attend follow-up appointments as recommended by your healthcare provider to monitor your liver health and ensure complete recovery.
- Vaccination: If not previously vaccinated, consider getting vaccinated against hepatitis A to prevent future infections.
- Precautions:
- Hygiene: Practice good hygiene, especially handwashing with soap and water after using the bathroom and before preparing or eating food, to prevent spreading the virus to others.
- Avoid Risky Behaviors: Practice safe sex and avoid sharing needles or personal items that could potentially spread hepatitis A.
- Educational Resources:
- Stay Informed: Learn more about hepatitis A, its transmission, and preventive measures to reduce the risk of future infections and protect others.
Psychological and Emotional Support:
Living with any illness can be challenging, and hepatitis A is no exception. It’s important to seek support from healthcare professionals, family, and friends if needed. Maintaining a positive outlook, following medical advice, and taking steps to maintain overall health can contribute to a smoother recovery and minimize the impact of hepatitis A on daily life.
Long-Term Outlook:
Most people with hepatitis A recover completely without long-term liver damage. However, individuals with pre-existing liver conditions or older adults may experience a more severe course of illness and require closer monitoring. With appropriate care and preventive measures, the risk of complications and recurrence of hepatitis A can be minimized.
Living with hepatitis A involves managing symptoms, supporting recovery through rest and nutrition, attending medical appointments for monitoring, and taking preventive measures to protect oneself and others from infection. With proper care and attention, most individuals can expect a full recovery and resume their normal activities without long-term health consequences.
Conclusion
In conclusion, hepatitis A is a viral liver infection that, while often mild and self-limiting, can present significant challenges during its acute phase. Characterized by symptoms such as jaundice, fatigue, and abdominal discomfort, hepatitis A typically resolves on its own without causing chronic liver damage in most cases. However, individuals with pre-existing liver conditions or older adults may be at greater risk of severe illness and complications.
Effective prevention strategies, including vaccination, practicing good hygiene, and being cautious with food and water sources, play a crucial role in reducing the incidence of hepatitis A. Prompt diagnosis, supportive care, and appropriate medical monitoring during the acute phase are essential for managing symptoms and ensuring recovery.
For those affected, living with hepatitis A involves prioritizing rest, hydration, and a nutritious diet while avoiding substances that may further stress the liver. Follow-up medical appointments and adherence to healthcare advice help monitor liver function and ensure complete recovery.
With proper management and preventive measures, individuals can typically expect a positive outcome and return to normal daily activities without long-term health implications. Education and awareness about hepatitis A are key to minimizing its impact on individuals and communities, emphasizing the importance of vaccination and hygiene practices in protecting public health.
