Glaucoma encompasses a range of conditions where damage to the optic nerve results in gradual vision loss. Typically associated with increased intraocular pressure, glaucoma can develop without noticeable symptoms until significant vision impairment occurs.
As a chronic condition, early diagnosis through regular eye exams and comprehensive understanding of risk factors are pivotal for effective treatment and management. Exploring its impact on vision health and advancements in therapeutic approaches underscores the importance of proactive eye care in combating this prevalent eye disease.
Table of Contents
Types of Glaucoma
Glaucoma encompasses several types, each characterized by different underlying causes, mechanisms, and clinical presentations. Understanding these variations is crucial for proper diagnosis, treatment, and management. Here are the main types of glaucoma:
- Primary Open-Angle Glaucoma (POAG):
- Description: POAG is the most common form of glaucoma, accounting for a majority of cases. It develops slowly over time as the drainage angle of the eye becomes less efficient, leading to increased intraocular pressure (IOP).
- Symptoms: Typically asymptomatic in the early stages, POAG can progress to peripheral vision loss (visual field defects) that may go unnoticed until significant damage has occurred.
- Risk Factors: Age, family history, African descent, and certain medical conditions (e.g., hypertension) are associated with higher risk.
- Angle-Closure Glaucoma:
- Description: Angle-closure glaucoma occurs when the iris blocks the drainage angle of the eye, leading to a sudden increase in IOP. This can be chronic (slowly progressive) or acute (sudden onset).
- Symptoms: Acute angle-closure glaucoma presents with severe eye pain, blurred vision, headache, nausea, and halos around lights. Chronic angle-closure glaucoma may have more subtle symptoms or be asymptomatic until advanced stages.
- Risk Factors: Hyperopia (farsightedness), older age, and anatomical variations in the eye structure predispose individuals to angle closure.
- Normal-Tension Glaucoma (NTG):
- Description: NTG is a form of open-angle glaucoma where optic nerve damage and vision loss occur despite normal IOP levels (typically considered less than 21 mmHg). The exact mechanisms are not fully understood.
- Symptoms: Similar to POAG, NTG is often asymptomatic until significant visual field loss occurs. Regular eye exams are essential for early detection.
- Risk Factors: Similar to POAG, but with emphasis on potential vascular or perfusion abnormalities contributing to optic nerve damage.
- Secondary Glaucoma:
- Description: Secondary glaucoma arises as a complication of other ocular or systemic conditions, such as trauma, uveitis (inflammation inside the eye), certain medications (e.g., corticosteroids), or tumors.
- Symptoms: Symptoms vary depending on the underlying cause but often include elevated IOP and visual disturbances.
- Treatment: Management focuses on treating the underlying condition and managing IOP as in primary glaucomas.
- Pigmentary Glaucoma:
- Description: Pigmentary glaucoma occurs when pigment granules from the iris accumulate in the drainage angle, obstructing the outflow of aqueous humor and leading to increased IOP.
- Symptoms: Typically affects younger adults, presenting with intermittent blurry vision, halos around lights, and elevated IOP.
- Risk Factors: Myopia (nearsightedness) and physical activities that cause rubbing or movement of the iris are associated risk factors.
- Congenital Glaucoma:
- Description: Congenital glaucoma is present at birth or develops shortly thereafter due to abnormalities in the development of the eye’s drainage system (trabecular meshwork).
- Symptoms: Excessive tearing, light sensitivity, and enlargement of the eye (buphthalmos) are common signs. It requires early diagnosis and surgical intervention to prevent irreversible vision loss.
- Treatment: Surgical procedures are often necessary to create a new drainage pathway or improve the existing one.
- Secondary Angle-Closure Glaucoma:
- Description: Unlike primary angle-closure glaucoma, this form occurs due to secondary factors such as intraocular tumors, inflammation (uveitis), or trauma.
- Symptoms: Similar to primary angle-closure glaucoma, symptoms may include sudden onset of severe eye pain, headache, blurred vision, and halos around lights.
Understanding the specific type of glaucoma a patient has is crucial for tailoring an effective treatment plan. Regular eye exams, awareness of symptoms, and early intervention are key to preserving vision and managing the progression of this sight-threatening disease.
Symptoms of Glaucoma
Glaucoma symptoms can vary depending on the type and stage of the disease. Importantly, in many cases, glaucoma may not cause noticeable symptoms until significant vision loss has occurred. Here are some common symptoms associated with different types of glaucoma:
- Primary Open-Angle Glaucoma (POAG):
- Often referred to as the “silent thief of sight” because it typically progresses slowly and without symptoms in its early stages.
- Peripheral vision loss: Initially, patients may notice blind spots in their side (peripheral) vision that gradually worsen over time.
- Central vision remains relatively preserved until advanced stages.
- By the time symptoms like halos around lights or blurred vision become noticeable, significant optic nerve damage has often occurred.
- Angle-Closure Glaucoma:
- Acute Angle-Closure Glaucoma:
- Chronic Angle-Closure Glaucoma:
- Gradual onset of symptoms, which may include mild eye discomfort or intermittent blurry vision.
- Similar symptoms to acute angle-closure glaucoma but less severe and may not be as noticeable.
- Normal-Tension Glaucoma (NTG):
- Symptoms are often similar to those of POAG because the optic nerve damage occurs despite normal intraocular pressure.
- Gradual loss of peripheral vision, which may go unnoticed until advanced stages.
- Central vision remains relatively clear until later in the disease.
- Pigmentary Glaucoma:
- Intermittent blurry vision, especially after physical activities that cause the iris to rub against the lens (e.g., exercise).
- Halos around lights, particularly noticeable in low light conditions.
- Elevated intraocular pressure (IOP) detected during routine eye exams.
- Congenital Glaucoma:
- Symptoms typically present in infants or young children:
- Excessive tearing (epiphora).
- Sensitivity to light (photophobia).
- Enlargement of the eye (buphthalmos).
- Cloudiness of the cornea.
- Squinting or closing one eye in bright light.
- Inability to fixate on objects or track moving objects.
- Symptoms typically present in infants or young children:
- Secondary Glaucoma:
- Symptoms vary depending on the underlying cause:
- Sudden or gradual increase in IOP.
- Blurred vision.
- Eye pain or discomfort.
- Redness of the eye.
- Vision loss related to the underlying condition (e.g., inflammation, trauma).
- Symptoms vary depending on the underlying cause:
Because glaucoma often progresses silently, regular comprehensive eye exams are crucial, especially for individuals at higher risk due to age, family history, or other predisposing factors. Early detection and treatment can help preserve vision and prevent irreversible damage to the optic nerve. If you experience any of these symptoms or have concerns about your eye health, it’s essential to consult an eye care professional promptly.
Causes of Glaucoma
Glaucoma primarily occurs due to damage to the optic nerve, often associated with elevated intraocular pressure (IOP). However, the exact causes of glaucoma can vary depending on the type of glaucoma. Here are the main causes associated with different types:
- Primary Open-Angle Glaucoma (POAG):
- Cause: The exact cause is not fully understood, but it is generally attributed to a combination of genetic predisposition and abnormalities in the eye’s drainage system (trabecular meshwork). This leads to reduced drainage of aqueous humor, causing a gradual increase in IOP and subsequent optic nerve damage.
- Angle-Closure Glaucoma:
- Cause: Angle-closure glaucoma occurs when the drainage angle of the eye becomes blocked, preventing the normal outflow of aqueous humor. This blockage can be caused by:
- Primary Angle-Closure: Anatomical variations in the eye structure, such as a shallow anterior chamber or a thickened iris, can predispose individuals to sudden closure of the drainage angle.
- Secondary Angle-Closure: This can result from conditions like cataracts, intraocular tumors, or inflammation (uveitis) that push or pull the iris forward, blocking the drainage angle.
- Cause: Angle-closure glaucoma occurs when the drainage angle of the eye becomes blocked, preventing the normal outflow of aqueous humor. This blockage can be caused by:
- Normal-Tension Glaucoma (NTG):
- Cause: The exact cause of NTG is not fully understood. It is hypothesized that vascular or perfusion abnormalities affecting the optic nerve may contribute to damage despite normal intraocular pressure levels.
- Pigmentary Glaucoma:
- Cause: Pigmentary glaucoma occurs when pigment granules from the iris detach and block the drainage angle of the eye, leading to increased IOP. This can be exacerbated by activities that cause mechanical rubbing of the iris against the lens, releasing more pigment.
- Congenital Glaucoma:
- Cause: Congenital glaucoma is present at birth or develops shortly thereafter due to abnormalities in the development of the eye’s drainage system (trabecular meshwork). It can be inherited or occur sporadically.
- Secondary Glaucoma:
- Cause: Secondary glaucoma results from other ocular or systemic conditions that impact the eye’s drainage system or increase IOP:
- Trauma: Injury to the eye can disrupt the drainage angle or increase production of aqueous humor.
- Inflammation: Uveitis and other inflammatory conditions can cause scarring and obstruction of the drainage system.
- Medications: Prolonged use of corticosteroid eye drops or systemic corticosteroids can increase IOP.
- Tumors: Intraocular tumors can physically block the drainage angle or increase IOP through other mechanisms.
- Other Factors: Certain systemic conditions like diabetes, hypertension, and vascular disorders may also contribute to glaucoma development.
- Cause: Secondary glaucoma results from other ocular or systemic conditions that impact the eye’s drainage system or increase IOP:
Genetics also play a significant role in many forms of glaucoma, with a family history of the disease increasing the risk of developing it. Additionally, age, race (African Americans and Hispanics are at higher risk), and certain anatomical variations in the eye structure can predispose individuals to glaucoma.
Overall, while elevated intraocular pressure is a common factor in many types of glaucoma, the precise mechanisms and causes can vary widely, highlighting the importance of regular eye exams and early detection for effective management and preservation of vision.
Risk Factors
Glaucoma risk factors can vary depending on the type of glaucoma but generally include a combination of genetic predisposition, age, and other health factors. Here are the key risk factors associated with different types of glaucoma:
- Age:
- Primary Open-Angle Glaucoma (POAG): Risk increases with age, particularly after 60 years old.
- Angle-Closure Glaucoma: Risk increases with age, but acute cases can occur at any age.
- Family History:
- A family history of glaucoma, especially in first-degree relatives (parents, siblings), increases the risk of developing glaucoma.
- Race/Ethnicity:
- Primary Open-Angle Glaucoma (POAG): People of African descent are at higher risk and may develop the condition at an earlier age.
- Angle-Closure Glaucoma: People of East Asian descent (Chinese, Japanese, Korean) are at higher risk due to anatomical predispositions.
- Intraocular Pressure (IOP):
- Elevated IOP is a significant risk factor for all types of glaucoma. However, normal-tension glaucoma (NTG) can occur with normal or even low IOP.
- Anatomy of the Eye:
- Angle-Closure Glaucoma: Anatomical variations such as a shallow anterior chamber or a narrow drainage angle increase the risk.
- Pigmentary Glaucoma: Myopia (nearsightedness) and activities that cause mechanical rubbing of the iris against the lens can increase risk.
- Medical Conditions:
- Systemic Diseases: Conditions like diabetes, hypertension, and cardiovascular diseases may increase the risk of developing certain types of glaucoma.
- Eye Conditions: Previous eye injuries, chronic inflammation (uveitis), and certain types of eye surgery may increase the risk of secondary glaucoma.
- Medications:
- Prolonged use of corticosteroids, whether as eye drops or systemic medications, can increase the risk of developing glaucoma (steroid-induced glaucoma).
- Other Factors:
- Gender: Some studies suggest that females may have a slightly higher risk of developing primary angle-closure glaucoma.
- Lifestyle Factors: Smoking and heavy alcohol consumption may increase the risk of developing glaucoma.
Understanding these risk factors can help individuals and healthcare providers identify those at higher risk for glaucoma and emphasize the importance of regular eye exams for early detection and management. Early diagnosis and treatment are crucial for preserving vision and minimizing the impact of glaucoma on daily life.
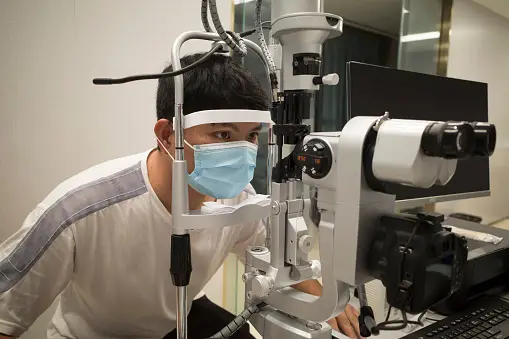
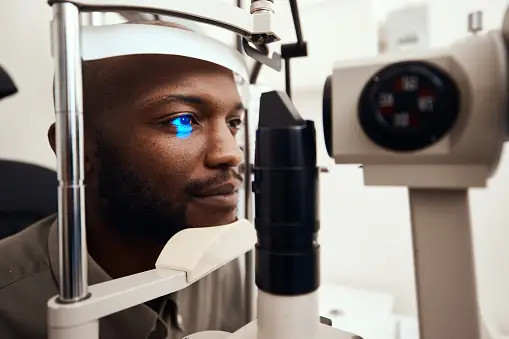
Diagnosis

Diagnosing glaucoma involves several key steps to assess optic nerve damage, measure intraocular pressure (IOP), evaluate visual field loss, and sometimes utilize imaging techniques to aid in diagnosis. Here’s an overview of the diagnostic process for glaucoma:
- Comprehensive Eye Examination:
- Visual Acuity: Testing how well you can see at various distances.
- Tonometry: Measuring intraocular pressure (IOP). Elevated IOP is a primary indicator but not always definitive for diagnosis.
- Gonioscopy: Examining the drainage angle of the eye to assess for any blockages or abnormalities that could lead to angle-closure glaucoma.
- Ophthalmoscopy: Examining the optic nerve at the back of the eye to detect signs of damage, such as cupping or thinning of the nerve fibers.
- Visual Field Testing:
- Perimetry: Mapping your visual field to detect any areas of vision loss, particularly in the peripheral vision. This helps identify patterns of damage caused by glaucoma.
- Imaging Techniques:
- Optical Coherence Tomography (OCT): Produces cross-sectional images of the retina and optic nerve head, helping to measure the thickness of nerve fibers. This can detect early signs of optic nerve damage even before visual field loss occurs.
- Gonioscopy: Direct visualization of the drainage angle of the eye to assess the risk of angle-closure glaucoma.
- Other Assessments:
- Pachymetry: Measurement of corneal thickness. Thinner corneas may indicate a higher risk of developing glaucoma.
- Visual Evoked Potential (VEP) or Electroretinography (ERG): These tests may be used in special cases to assess optic nerve function and response to visual stimuli.
- Evaluation of Risk Factors:
- Taking into account family history, age, race, and other health conditions that may predispose you to glaucoma.
Early detection and regular monitoring are crucial for managing glaucoma and preserving vision. If you experience any symptoms such as blurry vision, eye pain, or changes in peripheral vision, it’s important to see an eye care professional promptly. With timely diagnosis and appropriate treatment, the progression of glaucoma can often be slowed or halted, minimizing the risk of irreversible vision loss.
Treatment for Glaucoma

Treatment for glaucoma aims to reduce intraocular pressure (IOP) to prevent or slow down further damage to the optic nerve and preserve vision. The specific treatment plan depends on the type and severity of glaucoma, as well as individual factors such as age, overall health, and response to treatment. Here are the main approaches to managing glaucoma:
- Medications:
- Eye Drops: These are often the first-line treatment for glaucoma. They work by either decreasing the production of aqueous humor (fluid in the eye) or improving its drainage from the eye, thereby lowering IOP. Examples include prostaglandin analogs, beta-blockers, alpha agonists, and carbonic anhydrase inhibitors.
- Oral Medications: In some cases, oral medications may be prescribed to reduce IOP, especially if eye drops are insufficient or not tolerated well.
- Laser Therapy:
- Laser Trabeculoplasty: This procedure helps improve drainage of fluid from the eye by treating the trabecular meshwork. It is often used for open-angle glaucoma and can reduce the need for medications.
- Laser Peripheral Iridotomy (LPI): Used primarily for angle-closure glaucoma to create a small hole in the iris, allowing fluid to flow more freely within the eye and reducing IOP.
- Surgical Procedures:
- Trabeculectomy: This surgical procedure creates a new drainage channel in the eye to lower IOP. It is often recommended when medications and laser therapy fail to adequately control IOP.
- Glaucoma Drainage Implants/Shunts: Devices implanted into the eye to facilitate drainage of aqueous humor and reduce IOP, particularly in cases where trabeculectomy is not effective.
- Minimally Invasive Glaucoma Surgery (MIGS): Newer surgical techniques that aim to lower IOP with fewer complications and faster recovery times compared to traditional surgeries.
- Combination Therapy:
- In some cases, a combination of medications, laser therapy, and/or surgical procedures may be necessary to achieve adequate IOP control.
- Lifestyle and Self-Care:
- Regular Monitoring: Ongoing monitoring of IOP and optic nerve health through regular eye exams is essential to detect changes and adjust treatment as needed.
- Medication Adherence: Following the prescribed schedule for using eye drops or oral medications is crucial for effective management of glaucoma.
- Healthy Lifestyle: Maintaining a healthy diet, regular exercise, and managing other health conditions such as diabetes and hypertension can help manage glaucoma.
- Patient Education and Support:
- Understanding the condition, treatment options, and the importance of adherence to treatment plans.
- Regular communication with eye care professionals to monitor progress and address any concerns or changes in symptoms.
Early diagnosis and treatment are critical in managing glaucoma and preventing irreversible vision loss. It’s essential for individuals with glaucoma to work closely with their eye care team to develop a personalized treatment plan that meets their needs and helps preserve their vision over the long term.
Prevention
Preventing glaucoma primarily involves early detection, regular eye exams, and managing risk factors that may contribute to the development or progression of the disease. While some risk factors such as age and family history cannot be changed, there are proactive steps individuals can take to reduce their risk and potentially delay the onset or progression of glaucoma:
- Regular Eye Exams:
- Routine comprehensive eye exams are crucial, especially for individuals over the age of 40 or those with a family history of glaucoma. Early detection allows for timely intervention and management to prevent vision loss.
- Monitor Intraocular Pressure (IOP):
- High IOP is a significant risk factor for glaucoma. Regular monitoring through tonometry during eye exams can help detect elevated IOP early, even before symptoms occur.
- Know Your Risk Factors:
- Awareness of personal risk factors, such as age, family history, race (African descent), and certain medical conditions (diabetes, hypertension), can prompt proactive monitoring and early intervention.
- Maintain a Healthy Lifestyle:
- Exercise: Regular physical activity and cardiovascular exercise can help maintain overall health and potentially lower IOP.
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and omega-3 fatty acids may support eye health. There is some evidence suggesting that green leafy vegetables and foods high in antioxidants may have protective effects against glaucoma.
- Avoid Smoking: Smoking can increase the risk of developing certain types of glaucoma, so quitting smoking or avoiding exposure to secondhand smoke is beneficial.
- Manage Other Health Conditions:
- Control systemic conditions such as diabetes and hypertension, as uncontrolled blood sugar and blood pressure levels can increase the risk of glaucoma.
- Use Eye Protection:
- Protecting the eyes from injury can help prevent secondary forms of glaucoma. Wear safety glasses or goggles when participating in sports or activities that pose a risk of eye injury.
- Understand Medication Risks:
- Be aware of the potential side effects of medications, particularly corticosteroids, which can increase IOP. Discuss alternatives or adjustments with healthcare providers if needed.
- Educate Yourself and Others:
- Stay informed about glaucoma and its risk factors. Encourage family members, especially those with a family history of glaucoma, to undergo regular eye exams.
While these preventive measures cannot guarantee the prevention of glaucoma, they can help reduce the likelihood of developing the condition or slow its progression. Regular communication with an eye care professional is essential for personalized advice and monitoring, especially for individuals at higher risk or those with early signs of glaucoma. Early detection and proactive management are key to preserving vision and maintaining eye health over time.
Complications
Glaucoma, if not properly managed, can lead to several complications that can significantly impact vision and overall eye health. These complications may arise due to elevated intraocular pressure (IOP) or as a result of treatments aimed at managing glaucoma. Here are some potential complications associated with glaucoma:
- Vision Loss:
- The most significant complication of glaucoma is progressive and irreversible vision loss, primarily affecting peripheral vision initially and potentially leading to central vision loss in advanced stages.
- Damage to the optic nerve fibers, caused by increased IOP, results in gradual loss of vision over time. This damage is irreversible, highlighting the importance of early detection and treatment.
- Blindness:
- In severe cases where glaucoma progresses unchecked or is poorly managed, irreversible blindness can occur. This underscores the importance of regular monitoring and adherence to treatment plans.
- Decreased Quality of Life:
- Visual impairment from glaucoma can significantly impact daily activities such as driving, reading, and mobility, affecting overall quality of life.
- Vision loss can also lead to increased dependency on others for daily tasks and activities.
- Side Effects of Treatment:
- Medication Side Effects: Some glaucoma medications, such as eye drops, may cause side effects such as eye irritation, redness, blurred vision, or systemic effects if absorbed into the bloodstream.
- Surgical Risks: Procedures like trabeculectomy or glaucoma drainage implants carry risks of complications such as infection, bleeding, or failure to adequately control IOP.
- Laser Treatment Risks: Laser procedures, while generally safe, can cause transient increases in IOP or other rare complications.
- Secondary Conditions:
- Certain types of glaucoma, especially secondary glaucomas (e.g., neovascular glaucoma, uveitic glaucoma), may be associated with underlying systemic conditions or eye diseases that can further complicate treatment and management.
- For example, conditions like diabetes or uveitis can contribute to increased IOP and optic nerve damage, requiring coordinated management of both conditions.
- Psychological Impact:
- Coping with the diagnosis of a chronic eye condition like glaucoma can lead to stress, anxiety, or depression, particularly as the disease progresses and vision loss becomes more apparent.
- Support from healthcare providers, counselors, and support groups can be beneficial in addressing these emotional challenges.
- Complications from Angle-Closure Glaucoma:
- Acute angle-closure glaucoma can lead to sudden and severe symptoms, including intense eye pain, nausea, and vision loss. Prompt treatment is crucial to prevent permanent damage.
To mitigate these complications, early detection through regular eye exams, adherence to treatment plans prescribed by healthcare providers, and proactive management of associated risk factors are essential. Timely intervention can help slow the progression of glaucoma, preserve vision, and maintain overall eye health and quality of life.
Living With Glaucoma
Living with glaucoma involves ongoing management to preserve vision and maintain quality of life. Here are some key aspects to consider when living with glaucoma:
- Regular Eye Exams:
- Routine eye exams are crucial for monitoring intraocular pressure (IOP), assessing optic nerve health, and detecting any changes in vision. Frequency of exams will depend on the severity and type of glaucoma, typically ranging from every few months to annually.
- Medication Adherence:
- If prescribed eye drops or oral medications to lower IOP, it’s essential to use them as directed by your eye care professional. Skipping doses can lead to fluctuations in IOP and compromise the effectiveness of treatment.
- Lifestyle Modifications:
- Physical Activity: Regular exercise can help improve blood flow to the optic nerve and may contribute to overall eye health. Avoid activities that involve heavy lifting or strenuous exertion, which can increase IOP temporarily.
- Diet: A healthy diet rich in fruits, vegetables, and omega-3 fatty acids may support eye health. Some studies suggest that antioxidants and certain nutrients (like vitamin C, E, and zinc) may have protective effects for the eyes.
- Smoking: Avoid smoking or exposure to secondhand smoke, as smoking can increase the risk of developing certain types of glaucoma.
- Monitoring Vision Changes:
- Be vigilant about changes in your vision, such as blurry vision, halos around lights, or peripheral vision loss. Promptly report any new symptoms to your eye care professional for evaluation.
- Support and Education:
- Educate yourself about glaucoma, including its causes, treatment options, and potential complications. Understanding your condition can help you make informed decisions about your eye care.
- Joining support groups or connecting with others who have glaucoma can provide valuable emotional support and practical tips for managing the condition.
- Regular Communication with Healthcare Providers:
- Maintain open communication with your eye care team. Discuss any concerns or questions you have about your treatment plan, medications, or lifestyle adjustments.
- Keep track of appointments and follow-up visits to ensure continuity of care and monitor the progression of glaucoma.
- Protecting Your Eyes:
- Wear protective eyewear, such as safety glasses or goggles, when participating in activities that pose a risk of eye injury. Preventing eye trauma can help reduce the risk of secondary glaucoma.
- Psychological Well-being:
- Coping with a chronic eye condition like glaucoma can be challenging emotionally. It’s important to seek support from family, friends, or mental health professionals if you experience feelings of anxiety, depression, or stress related to your condition.
By actively managing your glaucoma through regular monitoring, adherence to treatment, and adopting a healthy lifestyle, you can help preserve your vision and optimize your overall eye health. Working closely with your healthcare team allows for personalized care and adjustments to your treatment plan as needed, enhancing your ability to live well with glaucoma.
Conclusion
Glaucoma is a chronic eye condition that requires lifelong management to preserve vision and maintain quality of life. With early detection, adherence to treatment plans, and proactive lifestyle adjustments, individuals with glaucoma can effectively manage the disease and minimize the risk of vision loss. Regular eye exams, medication adherence, and lifestyle modifications such as regular exercise and a healthy diet are essential components of glaucoma management.
Additionally, staying informed about the condition, seeking support from healthcare providers and support groups, and protecting the eyes from injury contribute to overall eye health. By taking these steps, individuals can navigate life with glaucoma with the goal of preserving vision and maintaining independence and well-being.
